A 38-year-old male presents to a community hospital emergency department at 3 a.m. and a rapid response is called to the front of the hospital. You respond, and the patient is alert but diaphoretic, weak, and displaying Levine’s sign (a fist clenched over his chest). His wife states that the chest pain started about 30 min prior to arrival. The patient is brought to your resuscitation bay, and his vital signs are as follows: BP 145/98, HR 99, RR 18, O2 93%. You ask for an EKG when then tech informs you that both of the EKG machines in the ED are broken, and we currently have no way of obtaining a tracing. What do you do in this scenario?
A Quick Review of ACS Metrics
Per the ACC/AHA [1,2], for non-PCI capable facilities:
PCI should be performed in patients with STEMI presenting within 120 minutes of first medical contact (Level B),
Fibrinolytic therapy should be administered in patients with STEMI transfer delay from first medical contact to PCI exceeds 120 minutes (Level B),
When fibrinolytic therapy is indicated as the primary reperfusion strategy, it should be administered within 30 minutes of hospital arrival (Level B).
Case: As this community site does not have PCI capabilities overnight, you are now on the clock and have 90 minutes remaining to get your patient to the appropriate location if this is an OMI. The EKG machines are still not working, and the inpatient charge nurses are called to try to find a working machine somewhere in the hospital.
Consider the Probe
In undifferentiated chest pain of suspected cardiac etiology, the focused cardiac ultrasound (FoCUS) exam is a useful tool to assess for cardiac pathology. This scope of this exam is regularly taught as assessing the 5 E’s of Echo: Effusion, Ejection, Equality, Entrance, and Exit.
The framework of the FoCUS exam is to provide protocol to ensure “consistent, deliberate, and systematic” assessment through the five sequential views: subcostal four chamber view (SC4C), subcostal view of the inferior vena cava (SCIVC), parasternal long axis view (PLAX), parasternal short axis view (PSAX), and apical four chamber view (A4C) [3].
These views allow for assessment of the E’s of echo:
SC4C → Pericardial effusion, Global LV/RV function,
SCIVC → Central venous pressure
PLAX → LV systolic function, LV/RV size, Pericardial effusion, Aortic assessment,
PSAX → LV systolic function, LV/RV size, LV segmental dysfunction,
A4C → LV/RV size, LV/RV systolic function, LV/RV diastolic function, LA/RA size.
Application of advanced bedside echocardiography techniques with tissue and transvalvular doppler increases the power of this exam with the ability to evaluate flow patterns that can help diagnosis stenosis, regurgitation, and acute versus chronic heart failure, among other pathologies.
Case: An immediate FoCUS exam was performed to assist with clinical decision making, which showed the following: HOTM FoCUS.MOV
This image demonstrates a regional wall motion abnormality (RWMA) in the left anterior descending artery (LAD) distribution (Figure 1). This RWMA can be visualized in multiple windows (PLAX, PSAX, A4C) but is best interpreted at multiple tissue levels of the PSAX view.
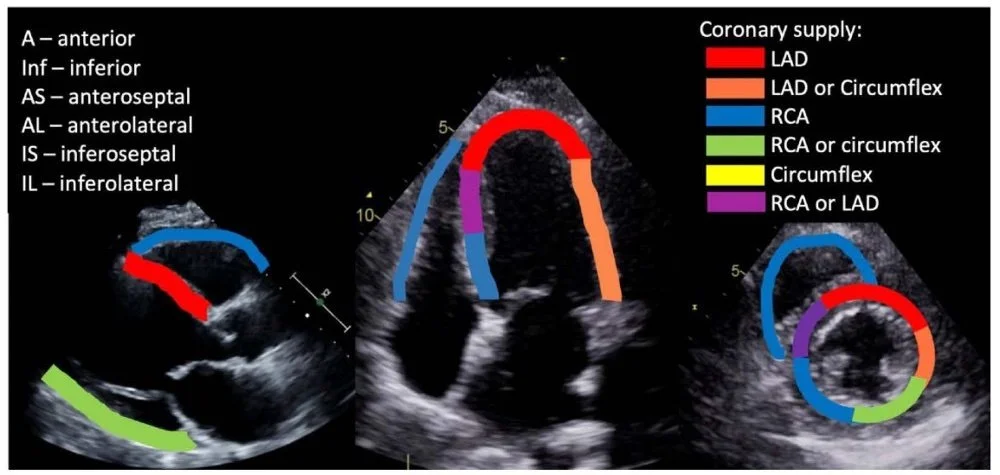
Figure 1. Coronary artery vascular distribution on FoCUS exam (Image from: https://asra.com/news-publications/asra-newsletter/newsletter-item/asra-news/2021/08/02/pocus-spotlight-focused-cardiac-ultrasonography)
Studies have demonstrated the Emergency Medicine physicians can rapidly diagnose RWMA and localize OMI with high diagnostic accuracy:
Croft et al., AJEM → Residents: Sensitivity 88%, Specificity 92% [4],
Bracey et al., AJEM,→ Residents Sensitivity 86%, Specificity 56%, Accuracy 77%; Fellows/Attendings Sensitivity 85% Specificity 75%, Accuracy 82% [5].
Case: EKG continues to be unavailable, and the decision is made to call for transfer to the nearest PCI center. The ultrasound images are sent to the cardiologist on call for review, and the transfer is accepted.
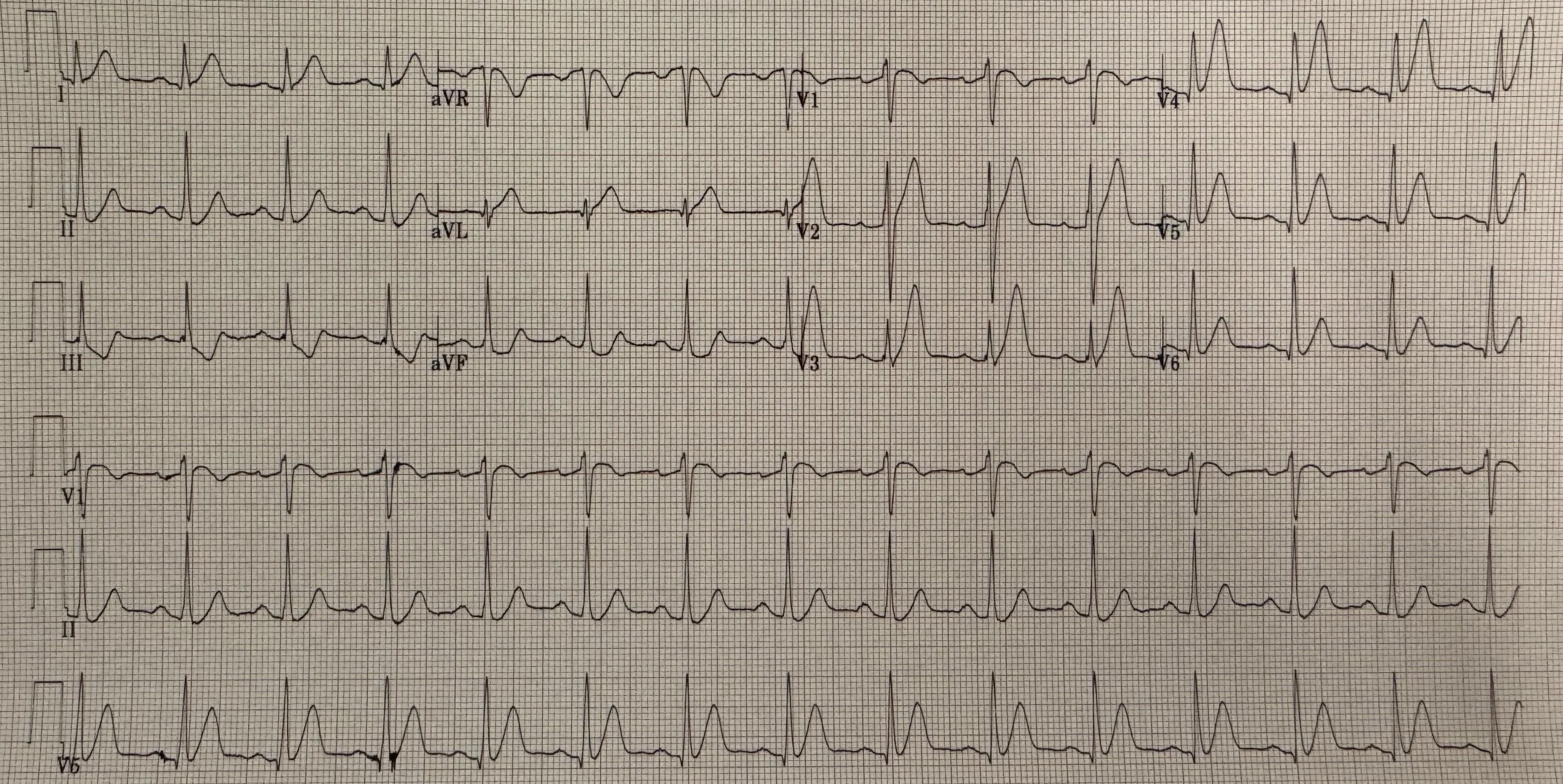
While the transfer is being set up, an EKG machine arrives from the ICU and the following is obtained (Figure 2):
Figure 2. Index EKG
Interpretation: Rate: 87; Rhythm: Normal sinus rhythm; Axis: Normal axis (I: pos, II: neg, aVF: pos); Intervals: PR: 178 (normal), QRS 94 (normal), QTc 413 (normal); P-waves: present; QRS Complex: normal; ST segment/T-waves: 2mm ST elevation in lead V1-V2, upsloping ST depressions with peaked T-waves in V3-V6
Case: This EKG confirms the findings of the FoCUS exam performed with ST changes consistent with ischemia in the LAD (anterior) distribution in leads V1-V2 with reciprocal changes in the inferior leads II, III, aVF & upsloping ST depressions with peaked T-waves in V3-V6. What is to be made of the upsloping ST depression in the LAD distribution?
The Heart of the Matter
The ST abnormality seen in the precordial leads of Figure 2 represents the de Winter T-wave pattern which is seen in only 2% of acute LAD occlusions [6]. De Winter’s is also known as “persistent hyperacute T-wave syndrome” and is defined by 1-3mm ST segment depression in leads V1-V6 with an upsloping ST segment continuing into hyperacute T-waves. Some individuals also demonstrate 1-2 mm ST-segment elevation in lead aVR, which is not observed in this patient’s EKG [7-8].
These findings highly suggest an acute coronary lesion and require emergent PCI. As such, it is important to recognize this pattern visually and not rely on biomarkers to make the diagnosis as cardiac biomarkers may initially be normal or only mildly elevated. Hyperkalemia can also mimic this EKG pattern and should remain on the differential, but consideration of this pattern for OMI mimic is critical for prompt diagnosis and treatment.
Interestingly, studies have shown that de Winter’s pattern is observed more in male and younger patients when compared to other individuals who present with an anterior OMI. Of note, the patient in this case was young (38 years old) and male [7].
Case: Ultimately, the patient was successfully transferred to a PCI-capable facility in under 45 minutes from initial presentation where he underwent angioplasty and DES placement for a 100% occlusive lesion of proximal to mid LAD.
Take Home Points
Ultrasound is powerful tool and can be used to convince our Cardiology colleagues to accept/treat a patient (e.g. Initiated and facilitated transfer in this case)
Utilize the FoCUS exam early in all patients with chest pain as it is rapidly available (often before EKG and Troponin) and has high diagnostic accuracy (77-82%)
If you see ST segment depression with upsloping hyperacute T-waves in the precordial leads, think de Winters pattern and OMI
References
2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: Executive Summary | Circulation
2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: Executive Summary | Circulation
FOCUS may detects wall motion abnormalities in patients with ACS, A retrospective study
Authored by Michael Hohl MD, David Murray MD, and Ari Edelheit MD