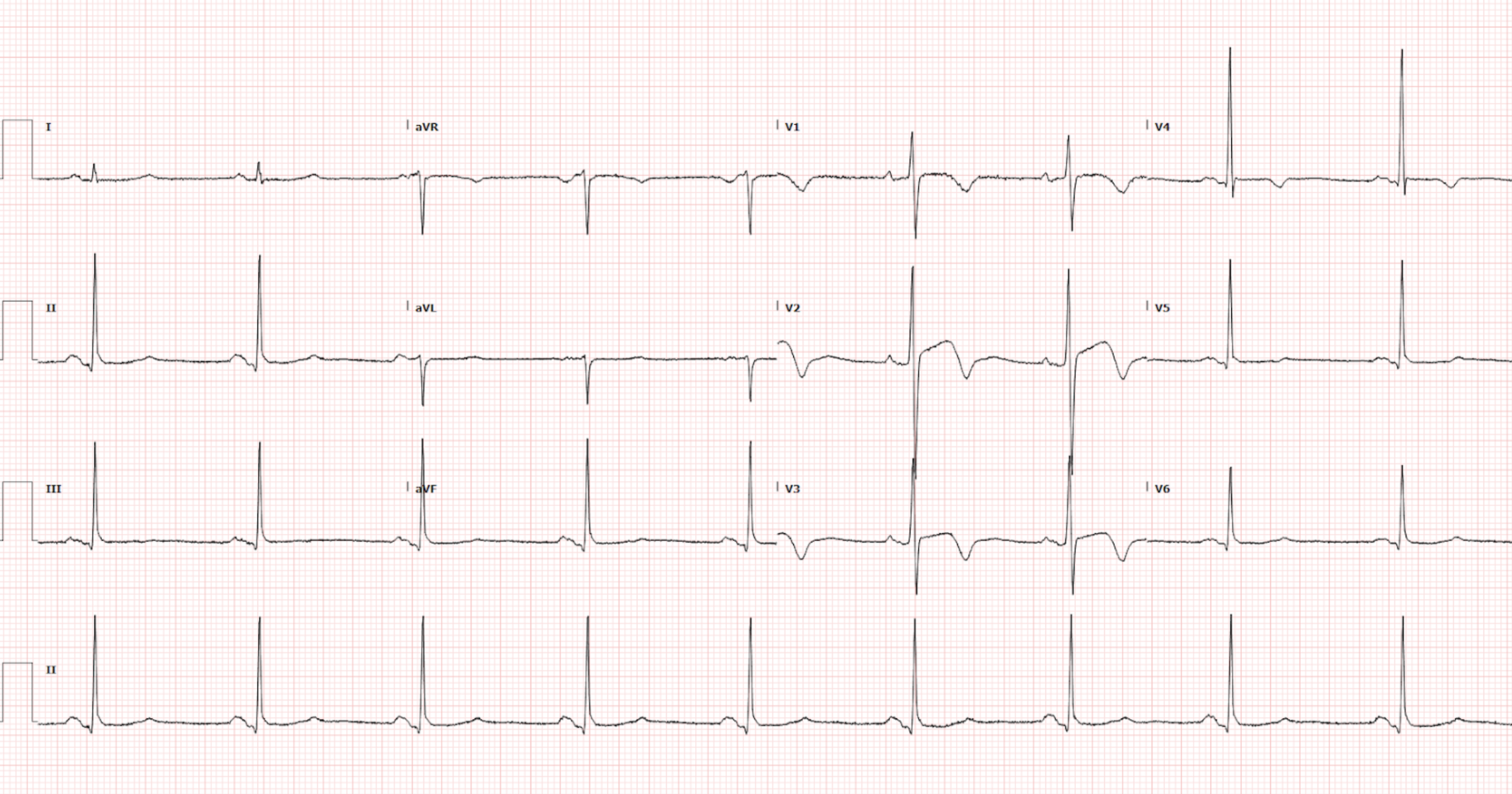
A 75-year-old female with a past medical history of atrial fibrillation on apixaban, bradycardia, depression, and anxiety presents for a fall. She had an unwitnessed syncopal event preceded by dizziness. The patient is brought into the trauma bay for evaluation.The patient is currently asymptomatic. Vitals signs are as follows: BP 142/65, HR 54, RR 14, SpO2 98% on room air, Temp 36.8C. You get an EKG (Figure 1).
Interpretation: Rate: 54 bpm; Rhythm: sinus bradycardia; Axis: normal (I: pos, II: pos, AVF: pos); Intervals: PR: 171 QRS: 88 QT: 454; P-waves: present, normal morphology; QRS complex: narrow; ST segment/T-waves: Inverted T-wave in V1, Biphasic T-waves in V2 and V3, inverted T-wave in V4
Laboratory testing was notable for a high-sensitivity troponin of 15 with an unchanged delta troponin and a BNP of 452. All other labs and imaging were unremarkable. The patient later experienced a sinus pause lasting greater than 3 seconds and cardiology was consulted. The patient was admitted to the CCU for further management.
Discussion
Now, it is ITE prep season and you all should be looking at this EKG and thinking: Syncope + Deep biphasic T-waves in the precordial leads + Mildly elevated troponin = …
This quick visual diagnosis should prompt you to think of Wellens Syndrome, an OMI equivalent. However, this EKG demonstrates a Wellens type A pattern. So what makes the difference between Wellens pattern and syndrome?
A Review of Wellens Syndrome (OMI Equivalent)
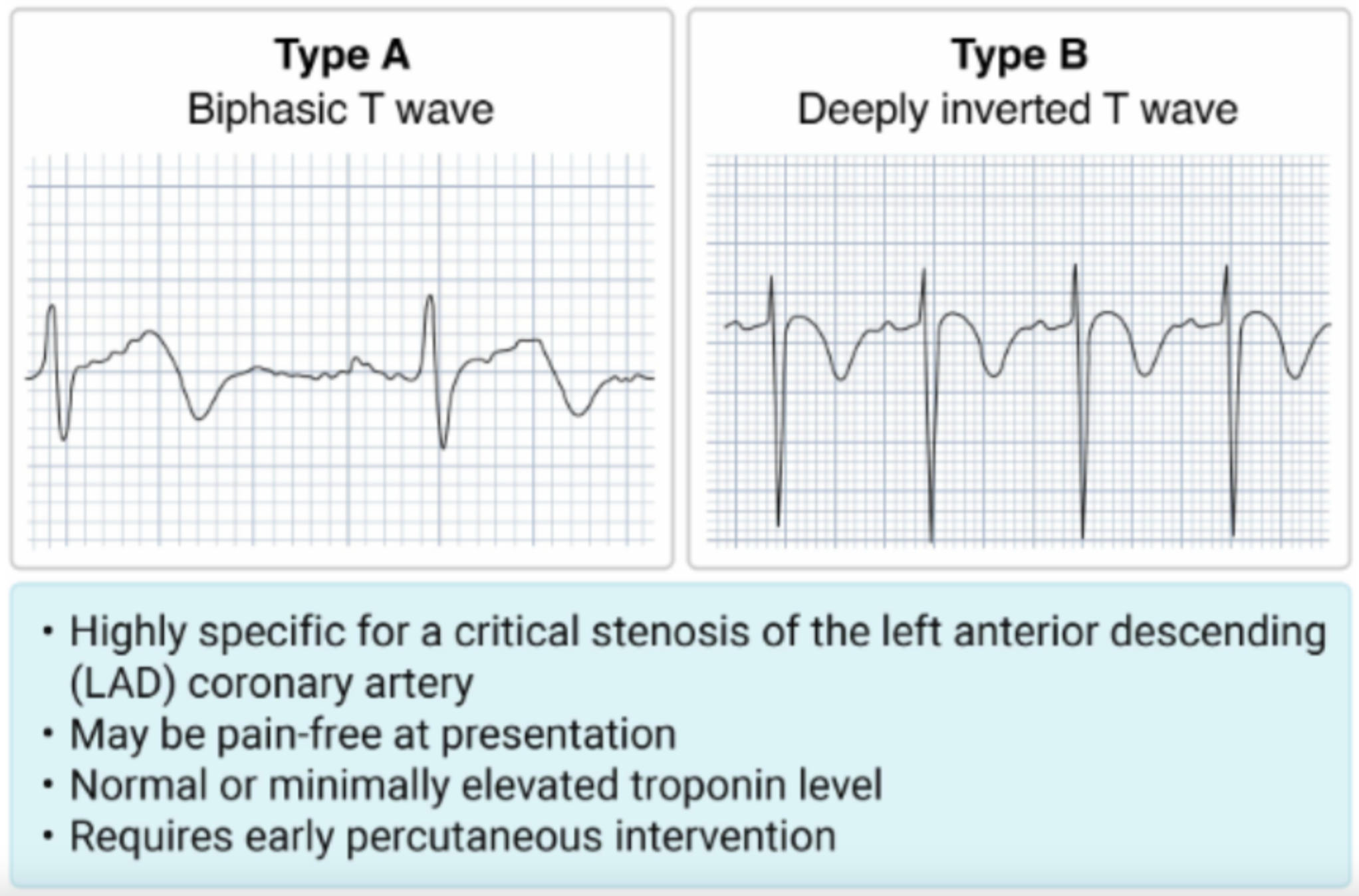
This syndrome is characterized by two phenotypes (Figure 2):
Type A: Biphasic T-waves in V2-V3; and
Type B: Deeply inverted T-waves in V2-V3.
Plus these additional criteria which must be met to be diagnostic for Wellens Syndrome:
No significant ST segment elevation (<1 mm)
No precordial Q waves, normal R wave progression (no evidence of old infarct)
Recent anginal chest pain
EKG changes present in a pain free state
Normal or only minimal elevation in troponin
Heart cath procedure showing critical stenosis of the left anterior descending.
Figure 2. Wellens Syndrome Phenotypes (Image from: https://www.roshreview.com/em/)
When these criteria are met, this pattern represents critical stenosis of the LAD and can lead to myocardial infarction in the weeks to follow [1]. Patients with this syndrome often will be pain free on presentation and may not present with the typical symptoms of ACS, though they usually will have experienced chest pain prior to arrival that has since resolved. Additionally, the majority of these patients will have negative cardiac enzymes, which again is falsely reassuring [2]. These EKG changes are a result of spontaneous reperfusion of the LAD. It is thought that this develops from a temporary obstruction of the LAD that resolves (by either lysis of the clot or other disruption) prior to true infarction, which explains the lack of symptoms on presentation and normal troponin. In fact, a similar EKG could be seen in a STEMI patient following successful percutaneous intervention of their LAD -- ST segments normalize and T-waves become biphasic or inverted as reperfusion sets in [3].
The mainstay of treatment for these patients is cardiac catheterization with revascularization. Research has shown that up to 75% of the patients who do not receive revascularization therapy with these EKG changes may develop extensive myocardial infarction. Thus recognition of these characteristic EKG changes as an emergency physician is critical [4,5]. Once recognized, aspirin and a cardiology consult is the name of the game as these patients will likely require stent placement.
The Wellens Mimic (Pseudo-Wellens)
As for our patient, she had a syncopal event and dizziness (a possible anginal equivalent), an EKG demonstrating biphasic T-waves in V2-V3 consistent with Wellens type A pattern, but did not have a cardiac catheterization performed to prove LAD stenosis. And, as such, she cannot be diagnosed with Wellens Syndrome in this case.
It is first important to note that pseudo-Wellens is a diagnosis of exclusion for the emergency physician. The first priority is to rule out OMI in every case where this pattern is detected and get cardiology onboard when in doubt. However, many conditions or states can mimic this pattern including:
Hypertension induced LVH [6],
Hypertrophic cardiomyopathy
Takotsubo’s cardiomyopathy,
Cocaine and/or Marijuana Use,
Coronary vasospasm or SCAD,
And even, acute cholecystitis [7,8].
So why did Cardiology not perform a cardiac catheterization on this patient?
The patient was found to have a history of recurrent sinus pauses detected on Zio patch monitoring from an outside hospital. Cardiology attributed the syncope to these pauses but recommended cardiac MRI to assess for structural heart disease in the setting syncope and biphasic T-waves which raises the possibility of HCM.
Moreover, always mind your medical evaluations when caring for your trauma patients, medical pathology can still occur, even in the Trauma Department. Patients who present for trauma may also have significant medical problems causing or contributing to their presentation and should receive BOTH a medical and trauma work-up :).
Take Home Points
Remember the two different phenotypes of Wellens Syndrome, in the correct clinical context, these findings are pathopneumonic for critical stenosis of the LAD :
Type A: Biphasic T-waves in V2-V3
Type B: Deeply inverted T-waves in V2-V3
Patients will be pain-free on presentation! Often demonstrating a normal troponin level
Do not let these patients walk out the door! Aspirin load and get cardiology consult asap for revascularization
References
de Zwaan Chris, Bär Frits W. H. M., Wellens Hein J. J. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. American Heart Journal. 1982;103(4):730–736. doi: 10.1016/0002-8703(82)90480-X.
Miner B, Grigg WS, Hart EH. Wellens Syndrome. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482490/
Cadogan, M., Buttner, R. and Buttner, M.C. and R. (2021) Wellens syndrome, Life in the Fast Lane • LITFL. Available at: https://litfl.com/wellens-syndrome-ecg-library/
Tandy TK, Bottomy DP, Lewis JG: Wellens’ syndrome. Ann Emerg Med March 1999;33:347-351.
Miner B, Grigg WS, Hart EH. Wellens Syndrome. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482490/
Ola O, Tak T. Pseudo-Wellens Syndrome in a Patient with Hypertension and Left Ventricular Hypertrophy. Am J Case Rep. 2019 Aug 20;20:1231-1234. doi: 10.12659/AJCR.916623. PMID: 31427564; PMCID: PMC6711489.
Migliore F, Zorzi A, Marra MP, Basso C, Corbetti F, De Lazzari M, Tarantini G, Buja P, Lacognata C, Thiene G, Corrado D, Iliceto S. Myocardial edema underlies dynamic T-wave inversion (Wellens' ECG pattern) in patients with reversible left ventricular dysfunction. Heart Rhythm. 2011 Oct;8(10):1629-34. doi: 10.1016/j.hrthm.2011.04.035. Epub 2011 May 10. PMID: 21699846.
Grautoff S, Balog M, Winde G. Pseudo-Wellens' syndrome and intermittent left bundle branch block in acute cholecystitis. Am J Emerg Med. 2018 Jul;36(7):1323.e1-1323.e6. doi: 10.1016/j.ajem.2018.03.081. Epub 2018 Apr 7. PMID: 29661666.
Authored by Auden Hafeman DO and Ari Edelheit MD