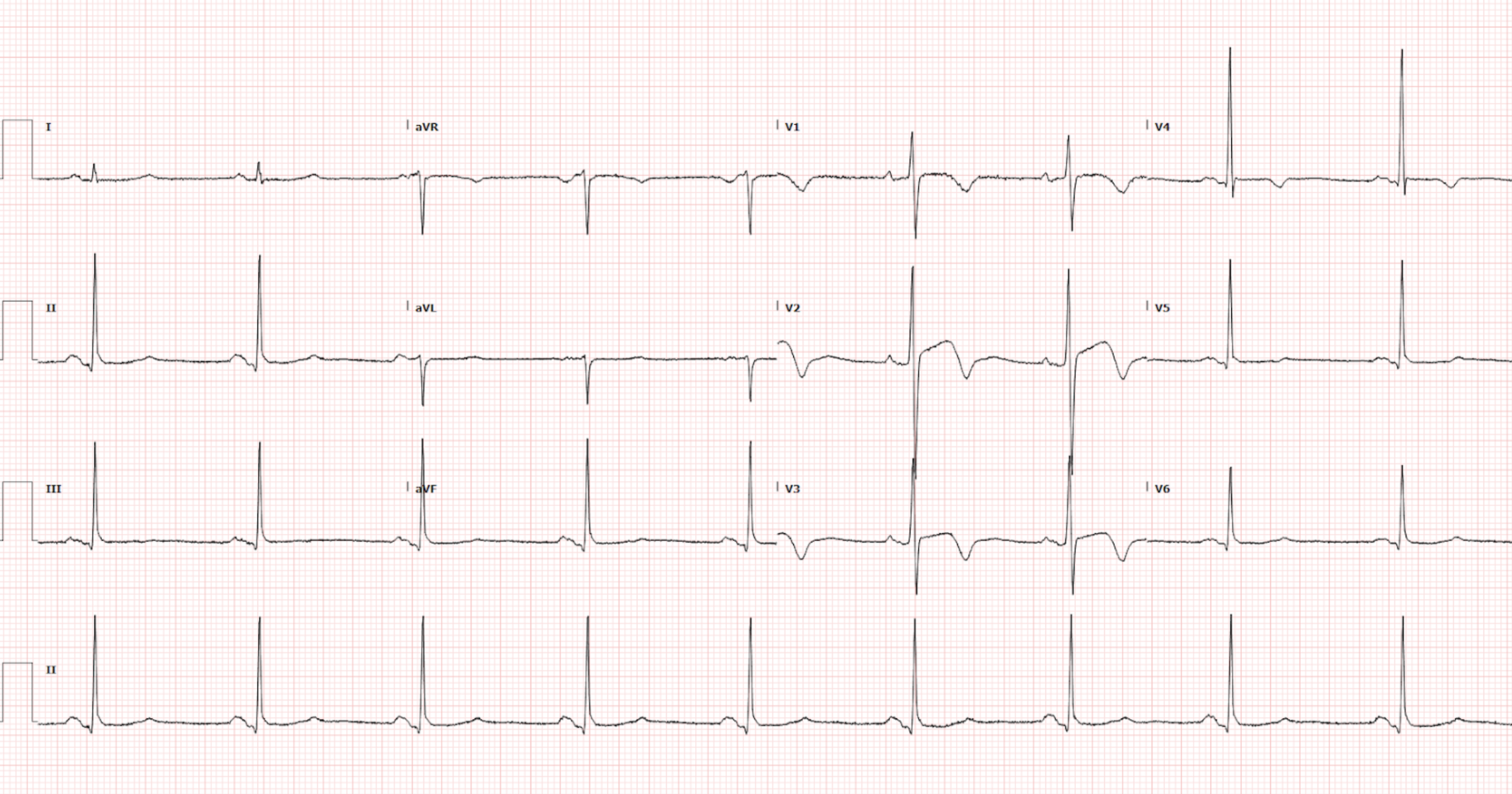
A 75-year-old female with a past medical history of atrial fibrillation on apixaban, bradycardia, depression, and anxiety presents for a fall. She had an unwitnessed syncopal event preceded by dizziness. The patient is brought into the trauma bay for evaluation.The patient is currently asymptomatic. Vitals signs are as follows: BP 142/65, HR 54, RR 14, SpO2 98% on room air, Temp 36.8C. You get an EKG (Figure 1).
Auden Hafeman DO and Ari Edelheit MD
Read More