A 56-year-old female with a past medical history of seronegative rheumatoid arthritis, fibromyalgia, hypothyroidism, and asthma presents to the emergency department for concern of "abnormal EKG" from the cardiology clinic. The patient states that she was previously told she has bradycardia and does endorse the occasional symptoms of palpitations, lightheadedness, and shortness of breath. She has a remote history of a stress test that was normal. The vital signs at time of assessment are shown: BP 151/74, HR 55, RR 20, O2 Sat 98% on room air. Laboratory testing in the emergency department is unremarkable and a chest x-ray showed no acute cardiopulmonary process. The patient had an EKG (Figure 1) completed in cardiology clinic.
Interpretation: Rate: 45 bpm; Rhythm: regular QRS complexes, regular p-waves; Axis: normal axis (I: pos., II: pos., aVF: pos) Intervals: PR: variable, appears very long, ~1.0-1.2s; QRS: 120, normal; QT: 400, normal; P-Waves: normal morphology; QRS Complex: normal, good R wave progression, delta wave in some complexes; ST Segment/T-waves: normal morphology, no elevation or depressions
Originally, when the patient was seen in Cardiology Clinic, the EKG was thought to be sinus bradycardia with 1st degree AV block given the apparent severe prolongation of the PR interval. However, this EKG actually demonstrates a complete heart block. Upon closer examination, there is evidence of buried P waves in the QRS complexes (the sometimes present delta wave) and the p-waves and QRS complexes march out at different but regular rates (Figure 2).
Figure 2. Index EKG with demarcated P-waves
This figure shows the P waves indicated by a red arrow. The sloping of the QRS complex is, in fact, not a delta wave, but a buried P wave. These findings are consistent with a diagnosis of complete heart block and after further review of the EKG, the patient was called into the emergency department for admission. The EKG on arrival to the emergency department (Figure 3) is shown below:
Figure 3. Repeat EKG in the Emergency Department
Interpretation: Rate: 66 bpm; Rhythm: irregular; Axis: left axis deviation (I: pos., II: neg., aVF: neg) Intervals: PR: variable; QRS: some narrow, some wide; QT: 450, normal; P-Waves: normal morphology; QRS Complex: intermittent LAFB, RBBB, narrow QRS, indicating possible junctional escape beats; ST Segment/T-waves: normal morphology, no elevation or depressions
This EKG is notably more complex to interpret. Cardiology interpreted this EKG as a 2nd degree Mobitz Type I Heart Block (Figure 4) with variable left anterior fascicular block (LAFB) and a right bundle branch block (RBBB). What supports this interpretation? When measured with calipers, there appears to be prolongation of the PR interval with each progressive p-wave followed by a dropped beat. However, these intervals are close but not exact which argues against this diagnosis. Additionally, only every fourth beat conducts with a morphology consistent with LAFB, indicating that these beats may be coming from alternating
ventricular escape foci from a multi-fascicle block rather than conducting from the p-waves as a Mobitz Type I.
Figure 4. Repeat ED EKG with PR intervals labeled and dropped beats indicated by blue arrows
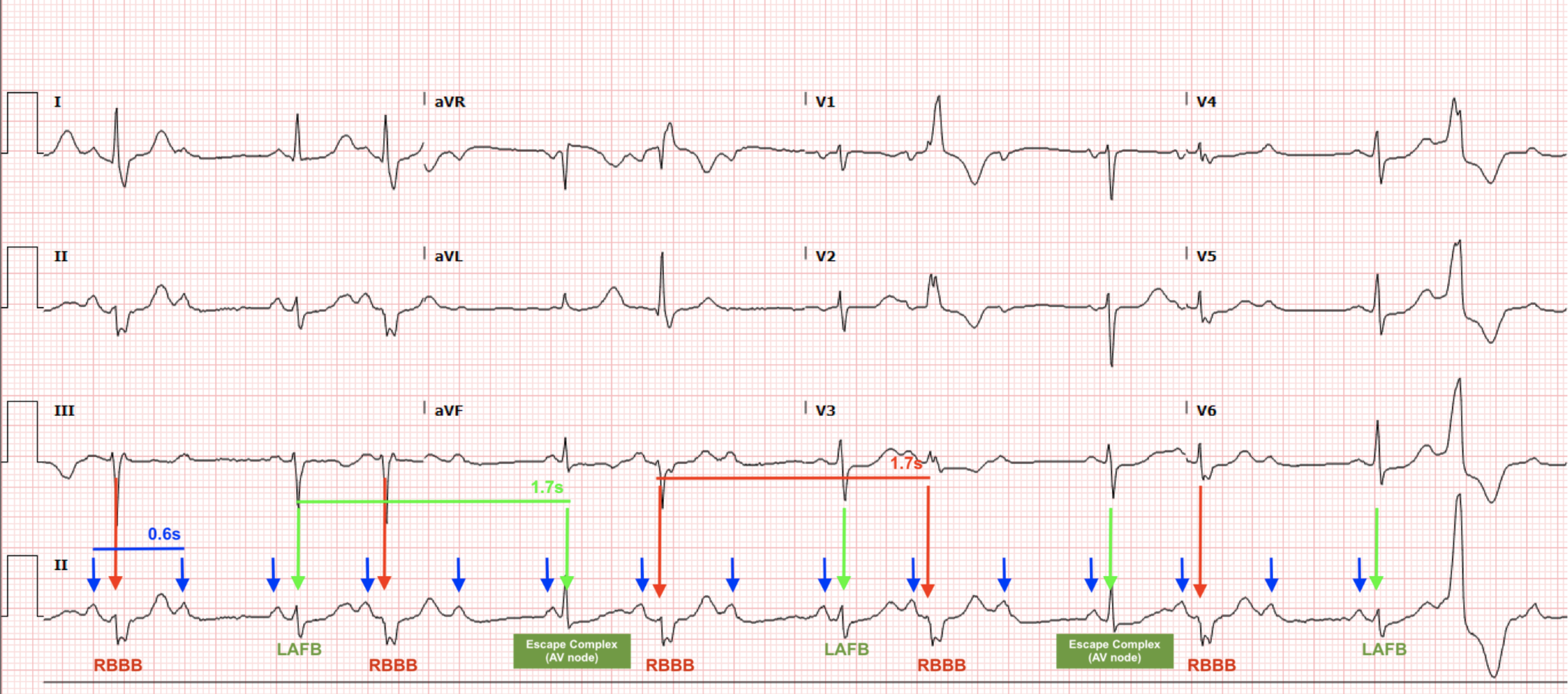
Our Heart of the Matter Team’s interpretation of this EKG is that this is still a 3rd degree complete heart block with junctional escape rhythms coming from the AV node (narrow complex QRS), left posterior fascicle (LAFB) and the left bundle branch (RBBB) due to an underlying, intermittent trifascicular block (Figure 5). The p-waves march out at a perfectly regular rate and the ventricular rhythm conducts independently at a slower but regular rate as well. We believe the overall EKG is still most consistent with complete heart block.
Figure 5. Index ED EKG with regular p-waves indicated by blue arrows, alternating but regular LAFB ventricular escape beats and AV node conducted narrow QRS complexes labeled by green arrows, and regular RBBB ventricular escape beats labeled by red arrows
The patient was ultimately admitted to the CCU for pacemaker placement with improvement in symptoms.
Discussion
Third Degree Heart Block (Complete Heart Block) results from complete dissociation of the SA and the AV node, leading to complete loss of coordination between the atria and the ventricles. Many times, this occurs from progression of a Second Degree Heart Block due to worsening of the patient’s disease [1].
This patient’s case highlights important points regarding ED treatment for higher degree heart block. Interestingly, the patient was noted to intermittently be in 1st, 2nd, and 3rd degree heart block on her EKGs and on the telemetry monitor in the CCU.
Operating under the assumption of Cardiology’s interpretation, the EKG from the emergency department (Figure 3) is showing a 2nd degree heart block with evidence of a high grade heart block given the associated RBBB and LAFB. This pattern is concerning for an impending trifascicular block. A trifascicular block happens when all three conducting systems distal to the AV node are failing, resulting in a RBBB, LAFB, LPFB and associated 3rd degree heart block [2].
Even without the prior EKG showing a complete heart block, a bifascicular block (Figure 3) in a symptomatic patient warrants admission to the hospital for cardiology consultation and likely pacemaker placement due to the high risk of development of trifascicular heart block with associated complete heart block [2].
Operating under the assumption of the HOTM Team’s interpretation, the EKG from the emergency department (Figure 3) is showing Complete Heart Block. In 3rd degree heart block, the atria are still controlled by the SA node, while the ventricles will conduct an escape rhythm. This rhythm can originate from the AV node, leading to a narrow complex QRS, or through an alternate pathway, leading to a widened QRS complex. In this case, we see a narrow QRS complex, so we can infer that this escape rhythm is mediated by the AV node, a LAFB complex (escape rhythm via the left posterior fascicle), and a RBBB complex (escape rhythm via the left bundle) [1,3].
This lack of communication between the SA and AV node can be caused by many different processes including: structural heart disease, ischemic etiologies, medications, electrolyte derangements, and also systemic diseases such as Lyme, amyloidosis, SLE and sarcoidosis for example. Our patient underwent a rheumatologic work-up that ultimately was negative [1,3]. Patients with complete heart block generally will be symptomatic, however the presenting symptoms can be vague such as fatigue, shortness of breath, pre-syncope and/or syncope. The degree of symptoms will be related to the rate of their ventricular rhythm, which normally will be less than 45-50 [1,3].
The EKG for a patient in complete heart block should have the following findings:
NO relationship between the P wave and the ORS complex
Atrial rate should be faster than the ventricular rate
QRS may be narrow or wide
There should be a regular P-P and QRS-QRS rate (Always be sure to look for extra “hidden” P waves in the QRS complexes and T waves)
Ultimately, the treatment for these patients is pacemaker placement. However, in the emergency setting there are multiple options for stabilization. Per ACLS guidelines, symptomatic bradycardia should be treated with atropine. However, in the case of a complete heart block, atropine is of minimal use as its primary mechanism functions at the level of the AV node, which is largely dysfunctional in these patients. Additional support can be garnered using the medications dopamine and epinephrine, which may improve heart rate in the acute setting. However, for patients both in high grade heart blocks and complete heart blocks who are unstable, the mainstay of treatment will be pacing, both transcutaneous and intravenous until they can get a permanent pacemaker implanted [1,3].
Take Away Points:
When you have a high suspicion for complete heart block, remember that the P-P ratio should remain consistent, and should be faster than the ventricular rate. Get out your calipers and go searching for buried P waves!
Regardless of the interpretation, the patient has a high degree AV block which ALWAYS needs to be admitted for pacemaker placement
Authored by Dr. Erica Dolph, Dr. Michael Hohl, and Dr. Ari Edelheit
References
Knabben V, Chhabra L, Slane M. Third-Degree Atrioventricular Block. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545199/
Buttner R, Larkin J. Trifascicular Block. In: Line in the Fast Lane. https://litfl.com/trifascicular-block-ecg-library/; 2023 Oct.
Buttner R, Larkin J. AV Block: 3rd Degree. In: Line in the Fast Lane. https://litfl.com/av-block-3rd-degree-complete-heart-block/; 2023 Nov.