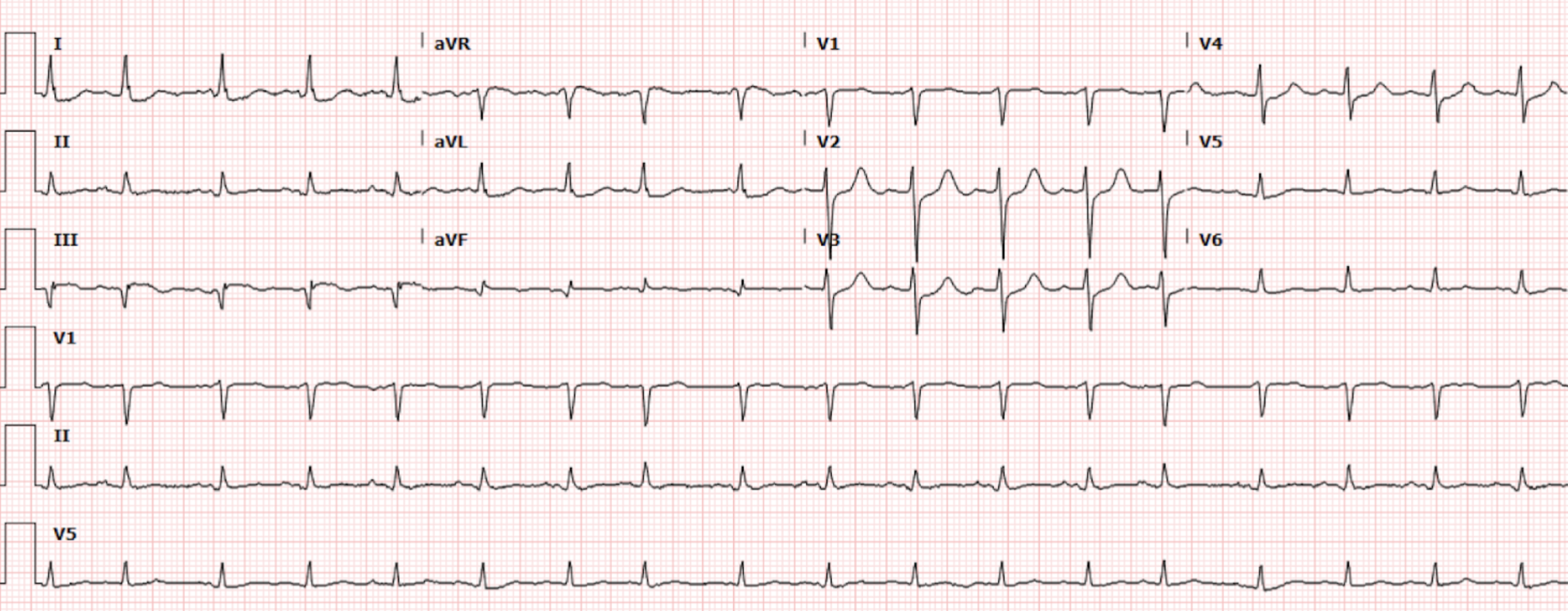
A 53-year-old man with no known medical history presents to the emergency department with three days of progressive shortness of breath and leg swelling. His dyspnea is worse with exertion. He denies chest pain, nausea, vomiting, or diaphoresis. Initial vitals notable for BP 190/95, HR 84, RR 24 and 86% on room air. The patient’s initial EKG (Figure 1) is shown.
Interpretation: Rate: 106 bpm; Rhythm: sinus rhythm Axis: normal axis deviation (I: pos, II: pos, aVF: pos) Intervals: PR: 175–normal; QRS: 76–normal; QTc: 396–normal; P-Waves: present QRS Complex: normal ST Segment/T-waves: ~0.75mm ST elevation in lead III, 0.5mm elevation in aVF, 1mm ST depression in lead I and aVL, 1mm ST depression in lead V2, V3 and V4
Our patients ECG findings are consistent with inferoposterior OMI. In the ED, patient was initiated on BIPAP, nitroglycerin drip and lasix for concern of acute decompensated heart failure and pulmonary edema. Labs notable for troponin elevated to 7.469 and BNP elevated to 1704. Cardiology was consulted for admission to CCU. At this point, EKG was obtained and showed STE elevation in lead III, avF concerning for inferior wall OMI therefore code STEMI was called. Left heart catheterization showed 100% thrombotic distal segment RCA occlusion. The patient underwent DES x2.
Discussion
This was undoubtedly a challenging case. Our patient presented with exertional dyspnea and signs of fluid overload consistent with new-onset acute decompensated heart failure. Although the differential diagnosis is broad, acute myocardial ischemia is one of the common precipitants and must be excluded. While our patient’s ECG does not meet classic STEMI criteria (>1 mm ST elevation in two contiguous leads), subtle electrocardiographic findings are present that are consistent with inferior and posterior occlusive myocardial infarction (OMI).
Inferior myocardial infarctions account for approximately 40–50% of all myocardial infarctions(MI) and generally have a more favorable prognosis than anterior MIs, with mortality rates typically below 10%. ST elevations are seen in inferior leads represented by leads II, III and aVF, with reciprocal changes seen in lead I and aVL. Lead aVL specifically is the only true lead electrically opposite to the inferior wall and therefore highly sensitive for inferior MI, showing up as ST depressions. Inferior infarctions typically result from occlusion of the dominant right coronary artery (RCA) in approximately 80% of cases, and less commonly from the left circumflex artery (LCx) in about 18% of cases. Greater ST elevation in lead III than II and/or STD in lead I and aVL suggests RCA as the culprit. RCA occlusion is further suggested by STE in V4R, seen in right-sided EKGs. On the other hand, ST elevation in lateral leads I and V5-V6 and lead II=III suggests LCx as the culprit. Although uncommon, the left anterior descending (LAD) can also be the culprit in an inferior infarction. These are called “type III’ or “wrap around” lesions and are defined by a pattern of inferior and anterior STE. Our patient EKG has ST elevation in III and aVF with concomitant reciprocal ST depressions in lead I and aVL that is highly suspicious for inferior OMI.
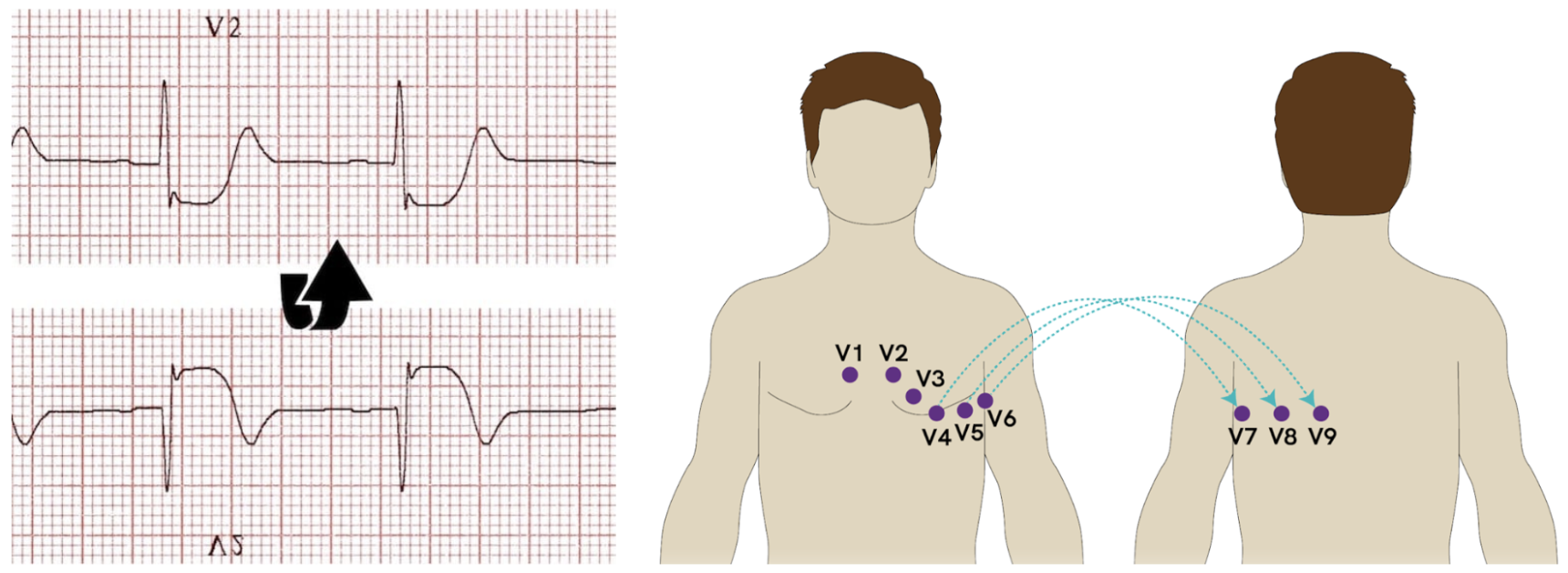
Posterior myocardial infarction accounts for approximately 15–20% of all myocardial infarctions and most commonly occurs as an extension of inferior or lateral MI. Isolated posterior MI is less frequently reported, likely because it is underrecognized on standard ECG, as it does not produce ST-segment elevation in the conventional leads. In standard EKG, reciprocal changes of ST elevations are seen in anteroseptal leads V1-V3 as anterior precordial leads are viewing the heart from the opposite (anterior) side of the injured posterior wall. This results in ST-segment depression and tall, broad R waves in V1–V3, findings that should raise suspicion for a posterior MI and prompt further evaluation with posterior leads V7–V9 (Figure 2). Posterior myocardial infarction occurs due to compromise of the posterior coronary circulation, most commonly involving the right coronary artery (RCA) or the left circumflex artery (LCx). Approximately 70% of individuals have right-dominant circulation, in which the RCA gives rise to the posterior descending artery (PDA) and supplies the posterior myocardium. About 10% have left-dominant circulation, with the PDA originating from the LCx, while the remaining 20% have codominant circulation, in which both the RCA and LCx contribute to posterior myocardial perfusion. Our patient EKG has ST depression in V2-V4 consistent with possible posterior circulation involvement in the infarction. Unfortunately posterior lead ECG were not obtained for this patient to confirm the diagnosis.
Figure 2. Posterior lead EKG (Image from: https://litfl.com/posterior-myocardial-infarction-ecg-library/)
Our patient was appropriately taken to the cath lab emergently for concern for posteroinferior myocardial infarction. Cath report was notable for 100% occlusion of the distal RCA which was the likely culprit of patients EKG changes and acute decompensated heart failure.
Take Home Points
In patients with acute decompensated heart failure, acute myocardial infarction must be ruled out
Evaluation of the inferior leads, together with reciprocal ST-segment depression in the high lateral leads (I and aVL) and the anterior leads (V1–V3), as well as changes in right-sided leads, is suggestive of an acute right coronary artery occlusion consistent with inferior and posterior myocardial infarction.
Primary ST depression in aVL with ST elevations in inferior leads is highly sensitive for inferior MI
If in doubt of OMI, do serial EKGs, POCUS and consider urgent cardiology consult
Sources
Buttner, E. B. (2024, October 8). Inferior STEMI. Life in the Fast Lane • LITFL. https://litfl.com/inferior-stemi-ecg-library/
Lizzo, J. M., & Shams, P. (2025, December 1). Posterior myocardial infarction. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK553168/
Burns, R. B. (2024, October 23). Posterior myocardial infarction. Life in the Fast Lane • LITFL. https://litfl.com/posterior-myocardial-infarction-ecg-library/
Tivakaran, V. S., & Rout, P. (2025, November 7). Inferior myocardial infarction. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470572/
Authored by Abish Kharel MD and Ari Edelheit MD