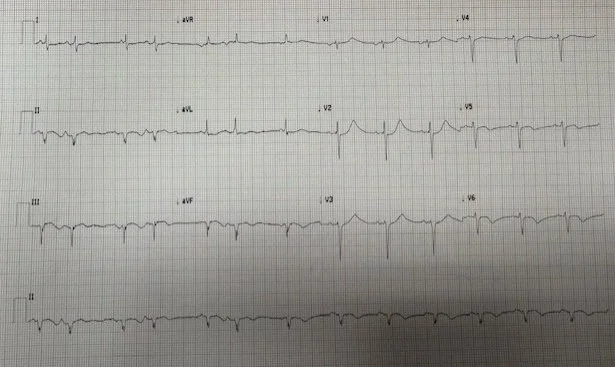
A 60-year-old male with hypertension and diabetes presented to the emergency department for two hours of substernal chest pain radiating to his jaw. The EKG from triage (Figure 1) is brought to the emergency physician (EP) stat due to some subtle abnormalities. Based on this EKG what are your next steps?
The EP brought the patient to the resuscitation bay and repeated the EKG in 5 minutes which demonstrated subtle findings but still did not meet STEMI criteria. Labs were ordered and the EP elected to obtain a 20 min repeat EKG (Figure 2).
Figure 2. Repeat EKG after 20 minutes
Based on this EKG, now, what are your next immediate steps?
Interpretation: Rate: 90 bpm; Rhythm: normal sinus rhythm; Axis: left axis deviation (I: pos., II: neg., aVF: neg) Intervals: PR: 137, normal ; QRS: 100, normal; QTc: 421, normal; P-Waves: present for every QRS; QRS Complex: bigeminal pattern; ST Segment/T-waves: 2mm ST depressions in V2-V5, new T-wave inversions in leads V4-V6, dynamic ST changes in lead II, III, aVF with 0.5mm ST elevation in Figure 1 and 2
A code STEMI was ordered immediately and the EP astutely obtained posterior leads (Figure 3) with demonstrated 2mm ST elevations in leads V4-V6. The troponin resulted at 11.4. Cardiology was consulted and the patient was prepped for left heart catheterization.
Figure 3. EKG with posterior leads
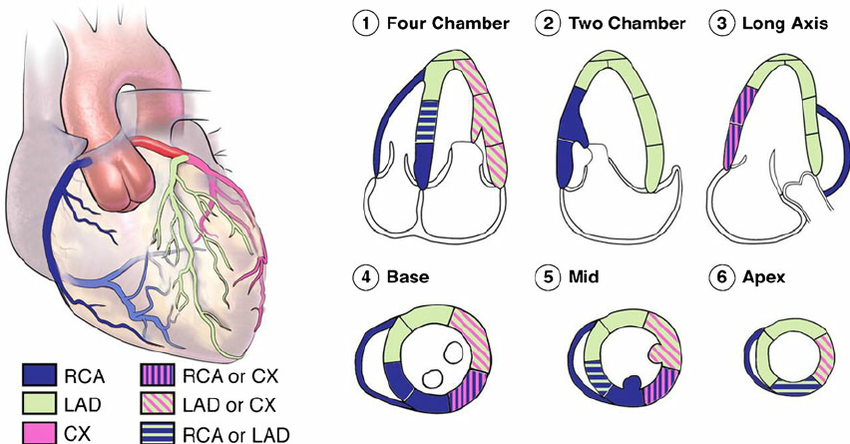
Prior to cath a comprehensive TTE was performed which showed left ventricular wall hypertrophy, ejection fraction of 50-55%, and a regional wall motion abnormality of the basalmid inferolateral and basalmid anterolateral myocardium.
The patient underwent the cath procedure and was found to have triple vessel disease with occlusions of 100% of the left anterior descending (LAD), 80% occlusion of the 1st diagonal (D1/LAD), 95% of the 1st obtuse marginal off the left circumflex (OM/LCx), 90% of the mid right coronary (RCA), and 100% of the right posterior descending (RPLS/RCA). Cardiothoracic surgery performed a quadruple coronary artery bypass grafting and the patient was admitted to the CCU for monitoring.
Discussion
Multivessel disease is defined as >70% stenosis of 2 or more coronary arteries, treatment for which can either be 1) medical management, 2) percutaneous coronary intervention (PCI) with placement of a drug eluting stent (DES), or 3) coronary artery bypass grafting (CABG). In the absence of OMI (e.g. NOMI, unstable angina), newer data suggests no difference in treatment between procedural intervention versus medical management, however there can be improvement in quality of life [1]. Notably, the SYNTAX Trail compared patients with triple vessel disease or left main disease who underwent either CABG or PCI with DES and found that at 1-, 3-, 5-, and 10-year intervals patient who underwent PCI had a significant hazard ratio for death compared to CABG (1.41, CI 95%) [2].
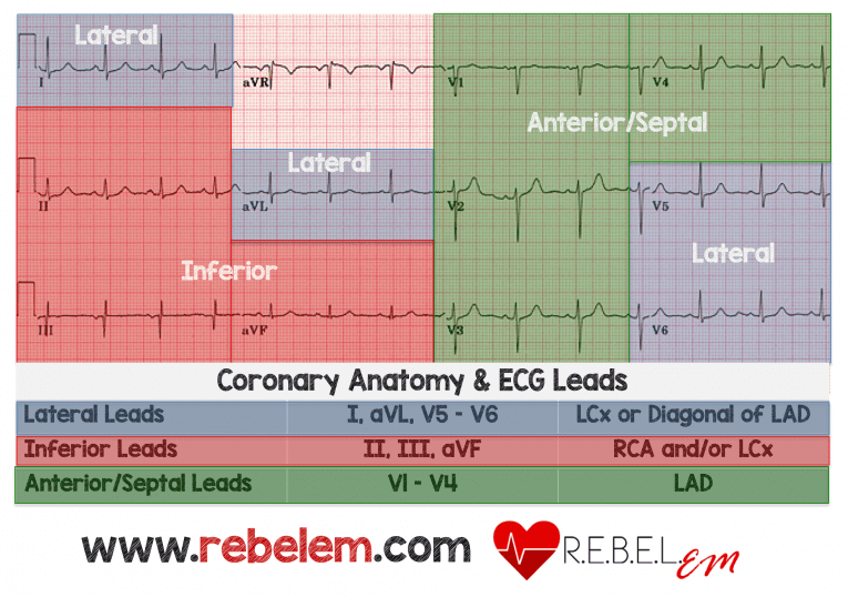
In this case the patient was found to have significant disease in the LAD (100%), RCA (90-100%), and LCx (80-95%). The vascular territories for these vessels on the EKG are shown below (Figure 4).
Figure 4. Coronary artery anatomy and EKG leads
Image from: https://rebelem.com/rebel-review/rebel-review-29-coronary-anatomy-ecg-leads/coronary-anatomy-ecg-leads/
Comparing Figure 2, Figure 3, and Figure 4, ischemic changes are observed occurring in the anteroseptal leads (LAD), the lateral leads (LCx), and the inferior leads (RCA). In Figure 2, there are 2mm ST depression in leads V2-V3, evidence of occlusive disease in the LAD, as well as 1mm ST elevations and biphasic T-waves in leads II, III, aVF, evidence of RCA disease. In Figure 3, there are 1-2mm ST elevation in leads V5-V6, evidence of LCx disease.
Furthermore, comparing these EKG findings to the TTE performed prior to catheterizations, again we see direct correlation between the RWMA–basalmid inferolateral (RCA) and basalmid anterolateral myocardium (LAD, LCx)–and the EKG (Figure 5).
Figure 5. Coronary artery anatomy and ultrasound vascular distribution
Take Away Points
If subtle but concerning abnormalities are present (think OMI/NOMI paradigm), continue to trend the EKG while waiting for troponin
If you have ST depression in V2-3 paired with ischemic changes in the lateral or inferior leads this is likely representative of an OMI (right coronary or left circumflex artery)
Early echocardiography can help identify RWMAs that localize to areas of subtle EKG changes and support your suspicion for OMI
Get an EKG with posterior leads (V7, V8, V9) when an posterior infarction is suspected. STEMI criteria for posterior leads are any one lead with 0.5mm ST elevation
References
Rossini R, Musumeci G, Navarese EP, Tarantini G. Coronary artery disease: to cath or not to cath? When and how best to cath: those are the remaining questions. Am J Cardiovasc Dis. 2013;3(1):27-38.
Thuijs DJFM, Kappetein AP, Serruys PW, et al. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial Lancet. 2019;394(10206):1325-1334. doi:10.1016/S0140-6736(19)31997-X
Gul F, Parekh A. Multivessel Disease. [Updated 2023 Feb 8]. In: StatPearls [Internet]; Jan 2025. Available at: https://www.ncbi.nlm.nih.gov/books/NBK557895/
Authored by Michael Hohl MD and Ari Edelheit MD