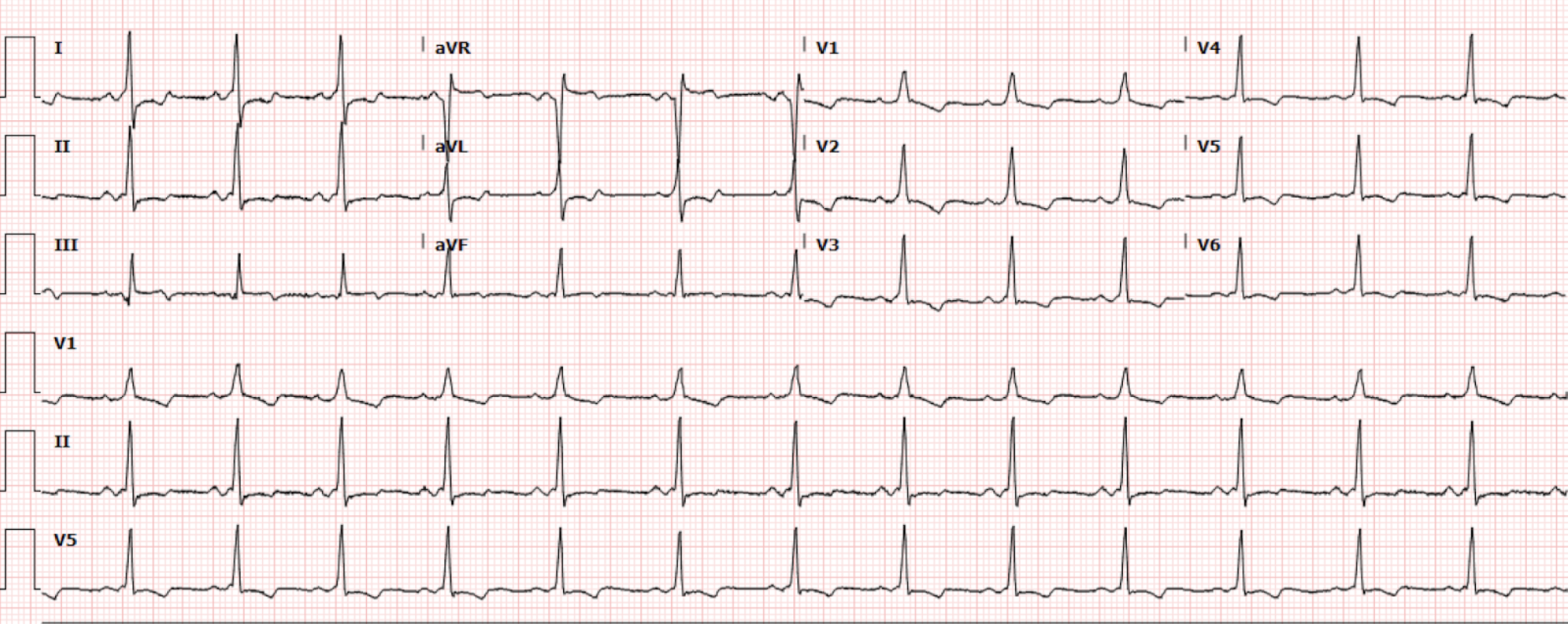
A 25-year-old male with no medical history presents to the emergency department with intermittent chest pain and palpitations. The chest pain is not exertional, positional, or radiating and the patient denies shortness of breath or syncope. The patient does note palpitations associated with lightheadedness.. He denies family history of sudden cardiac deaths. Initial vital signs are notable for BP 129/58, HR 76, RR 18, and O2 saturation of 98% on room air. The patient’s initial EKG (Figure 1) is shown.
Interpretation: Rate: 81 bpm; Rhythm: sinus rhythm Axis: normal axis deviation (I: pos, II: pos, aVF: pos) Intervals: PR: ~110-120 narrow ; QRS: 120ms-wide; QTc: 369–normal; P-Waves: present QRS Complex: wide complex with delta wave ST Segment/T-waves: 0.5mm ST depressions in anterior leads I, avL, V1-6, mild ST elevation III, aVF; T wave inversions V1-V6
In the ED, initial troponin 0.025, repeat 0.023. On close inspection of this EKG, there are findings consistent with a pre-excitation syndrome, or Wolff-Parkinson-White (WPW). Cardiology was consulted and recommended admission for EP study and possible ablation. Ultimately, the patient received ablation with the Electrophysiology (EP) team and was found to have a left lateral accessory pathway at 1 o’clock position on the mitral valve annulus. The post procedure EKG (Figure 2) showed no pre-excitation indicating successful ablation therapy.
Figure 2. Post-ablation EKG
Discussion
Wolf-Parkison White Syndrome is caused by the presence of a congenital accessory pathway between the atria and ventricles. Conduction via the accessory pathway bypasses the AV nodal delay and pre-excites, or slow depolarizes, the ventricle which leads to a slurred, or slow, upstroke of QRS rather than a fast upstroke as is seen in normal QRS complexes conducted by the AV nodal-His-Purkinje system. Accessory pathways are formed during cardiac development and can exist in variable locations.
The hallmark EKG findings of WPW consist of a short PR interval (<120ms) and a prolonged QRS (>110ms) with a slurred upstroke of the initial portion of QRS wave, referred to as the delta wave.
In WPW, the accessory pathways predispose different forms of tachyarrhythmias (Figure 3):
Orthodromic reentrant tachycardia
Orthodromic AV Reentrant Tachycardia is the most common type.
Impulse travels down the AV node and returns up the accessory pathway which produces a narrow complex tachycardia.
Antidromic AVRT
Impulse travels down the accessory pathway and back up the AV node which produces a wide complex tachycardia.
Atrial fibrillation/Atrial flutter with WPW
Atrial fibrillation conduction rapidly conducts to the ventricles via the accessory pathway. With no protective AV nodal delay, this rhythm can progress into rapid irregular wide complex tachycardia with significant risk of ventricular fibrillation and sudden cardiac death.
Figure 3. Orthodromic vs Antidromic WPW
Patients with WPW pattern can be asymptomatic if they have not developed a tachyarrhythmia. Those with tachyarrhythmias will often develop symptoms such as chest pain, lightheadedness and dyspnea. In general, young healthy patients with asymptomatic WPW patterns can be referred for outpatient workup with cardiology.
Patients who are at higher risk (age, cardiac risk factors, symptoms, comorbidities) should be discussed with cardiology upon discovery of WPW for either close follow up or in-hospital EP work-up. Patients who are acutely presenting with tachyarrhythmias with WPW pattern or prior symptomatic episodes, even without a present tachyarrhythmia, require urgent intervention with medical management and ablation.
In the emergency department, acute tachyarrhythmias with WPW or history of WPW require acute medical management. ACLS tachyarrhythmias guidelines should be followed to stabilize these patients. Unstable patients (hypotension, altered mental status, shock) should undergo synchronized cardioversion.
In stable patients with acute tachyarrhythmias with WPW pattern or in patients with history of WPW, the pharmacological treatment of choice varies depending on tachyarrhythmia. For orthodromic AVRT (narrow complex), treatment of choice is similar to other SVTs, including vagal maneuvers and adenosine. AV nodal blockers such as adenosine can be trialed given conduction is via AV node, not the accessory pathway. For antidromic AVRT (wide complex), the treatment of choice is procainamide. AV nodal agent blockers (such as adenosine, beta blockers) should be avoided as it promotes conduction down accessory pathways increasing risk of ventricular fibrillation. Similarly in atrial fibrillation/atrial flutter with WPW, treatment of choice is procainamide. AV nodal agents should be avoided for the same reason as above.
Take-way points:
Symptomatic WPW predisposes patients to life-threatening tachyarrhythmias therefore should be discussed with cardiology for definitive management with ablation
Acute tachyarrhythmias with WPW requires urgent medical management dependent on rhythm. If unclear on rhythm, AV nodal agents should be avoided.
A lot of times we don't know a narrow complex tachycardia is from orthodromic AVRT until after the patient is cardioverted (chemically or electrically). This is why it is so important to get post-conversion ECGs for patients!
References:
Chhabra L, Goyal A, Benham MD. Wolff-Parkinson-White Syndrome. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan
Burns, Ed, et al. “Pre-Excitation Syndromes.” Life in the Fast Lane • LITFL, 29 Aug. 2025,
Rawshani, Dr Araz. “Pre-Excitation, Atrioventricular Reentrant (Reentry) Tachycardia (AVRT) and Wolff-Parkinson-White (WPW) Syndrome: ECG, Clinical Characteristics and Management.” Kardiovaskuläre Medizin Online, 22 Jan. 2021
Authored by Abish Kharel MD and Ari Edelheit MD