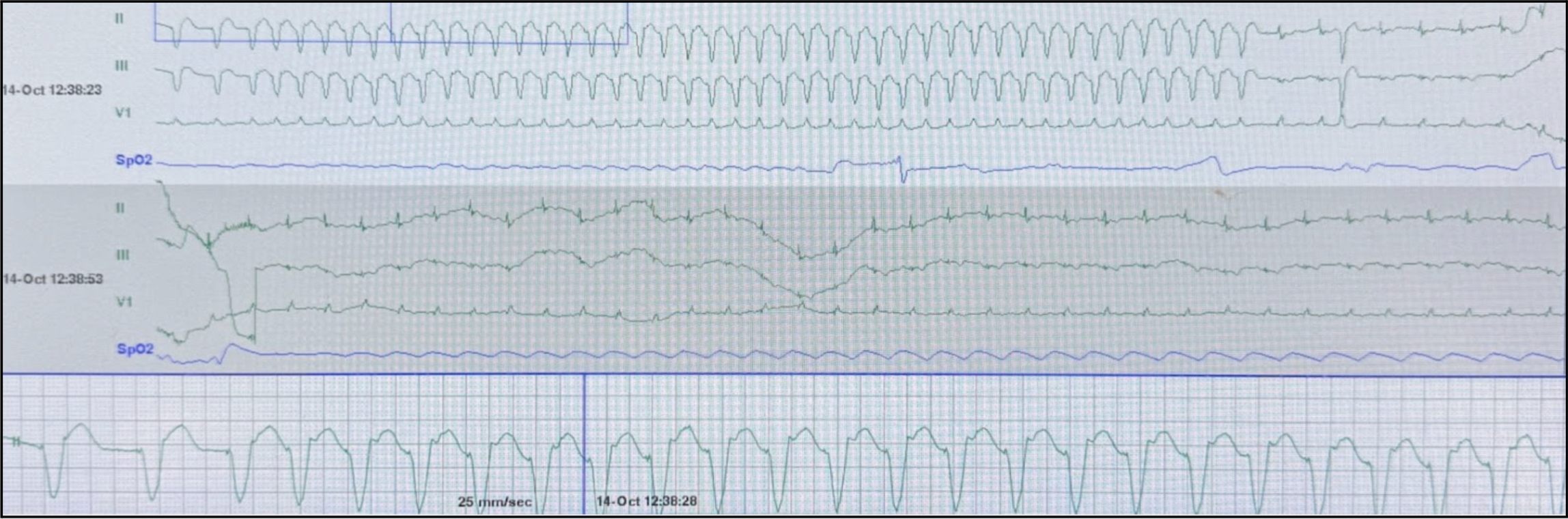
A 74 year old male with history of STEMI s/p PCI with DES of LAD and RI, HFrEF (EF 20-25%), sick sinus syndrome s/p DC-PPM, atrial flutter, hypertension, insulin-dependent diabetes, severe PAD s/p right IR SFA stent, and pancreatic insufficiency presenting for hypotension from general surgery clinic. The patient is brought to the resuscitation bay and while you are waiting for your work-up the monitor alarms and shows the following (Figure 1).
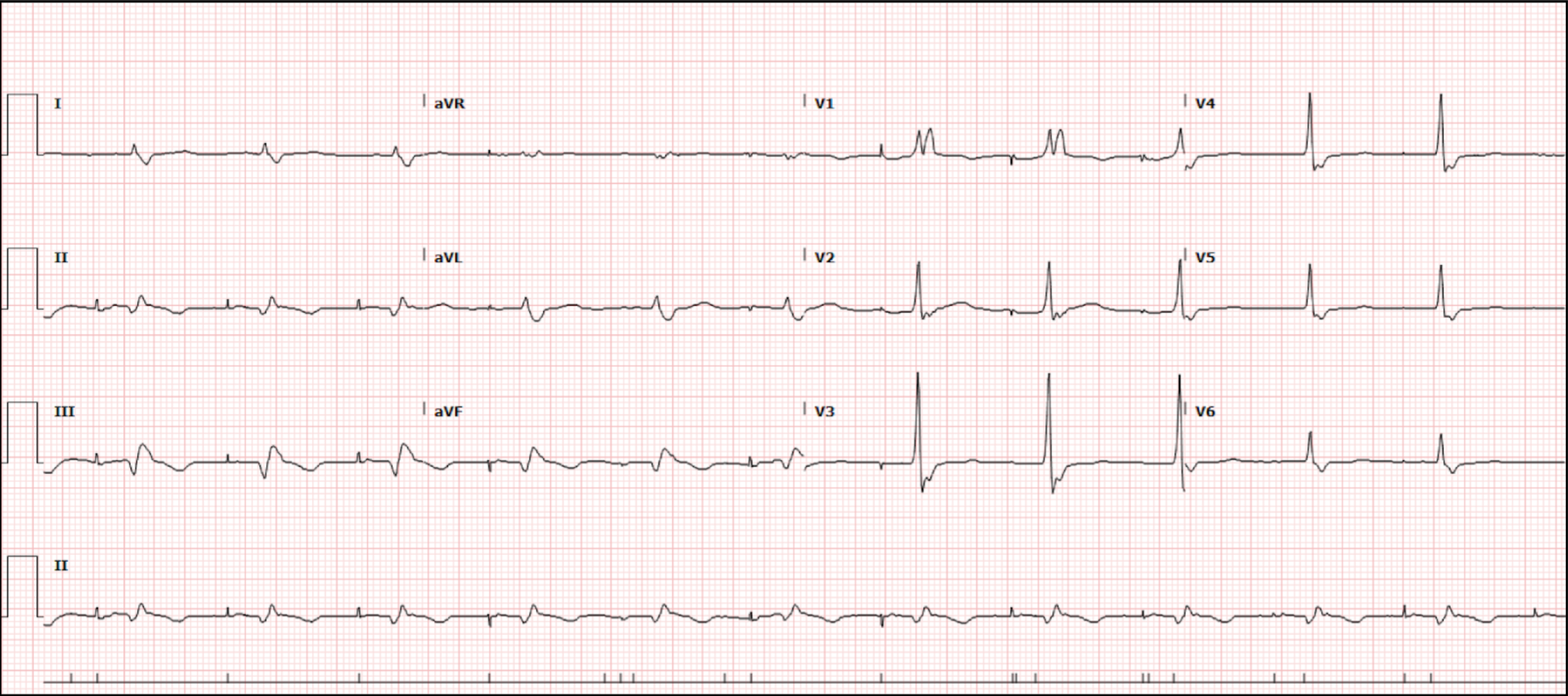
A stat EKG is ordered (Figure 2) which shows the following:
Figure 2. Index EKG
Given the patient’s cardiac history, what is your differential for this non-sustained wide complex tachycardia?
Discussion
The patient in this case has multiple medical conditions that predispose him to developing a wide complex tachycardia, including:
STEMI → ventricular tachycardia
Atrial Flutter → aberrancy
Sick Sinus Syndrome → supraventricular tachycardia with aberrancy
DC-PPM Placement → pacemaker mediated tachycardia
Pancreatic Insufficiency → hypocalcemia, hypokalemia, hypomagnesemia
So, how was the diagnosis made? When looking closely at Figure 1, we notice what appears to be retrograde p-waves appearing just after the wide QRS complex (Figure 3).
Figure 3. Telemetry strip with arrows indicating retrograde p-waves
When considering the native rhythm seen in Figure 2, paced sinus rhythm with RBBB, and the arrhythmia of wide complex tachycardia with retrograde p-waves seen in Figure 1, this highly supports the diagnosis of pacemaker mediated tachycardia (PMT). PMT is a re-entrant tachycardia where the pacemaker forms the anterograde pathway and the native pathway through the AV node forms the retrograde pathway, creating an endless-loop, similar to antidromic AVRT [1]. This antidromic loop results in the observed retrograde p-wave after ventricular depolarization as the atria are depolarized after the ventricles via the native retrograde pathway.
This arrhythmia is mediated via pacemaker sensing of retrograde p-waves as native atrial depolarizations resulting in continuous and accelerating ventricular depolarization via the pacemaker. However, the tachycardia is inherently limited by the programmed rate of the pacemaker [2].
Treatment for PMT is simple: place a magnet of the pacemaker to turn on fixed pacing. Alternatively adenosine can be used to slow down AV nodal conduction (unlike in antidromic AVRT).
So, how was the patient treated in this case? Electrophysiology was consulted and ultimately changed the rate-responsive post-ventricular atrial refractory period (PVARP) from low to high. The PVARP is defined at the programmed timeframe following a ventricular heartbeat (either natural or paced) during which the pacemaker's atrial lead is "blind" and cannot sense or respond to any atrial signals [3]. This helps prevent sensing of retrograde p-waves as native beats and causing an accelerating PMT. Rate-responsive PVARP allows for automatic shortening of the PVARP at high native heart rates to better track faster atrial rhythms and lengthening of the PVARP to avoid sensing the retrograde p-wave when PMT is detected.
Take Away Points
Pacemaker mediated tachycardia is a ventricular tachycardia mimic and can most safely be treated with a magnet prior to giving medications (especially if the diagnosis is still unclear)
If magnet termination fails, consider alternative diagnoses other than PMT
If a magnet is unavailable, adenosine can be used to slow down conduction via the AV node and terminate the re-entry circuit arrhythmia
References
Burns E, Buttner R, Buttner EB and R. Pacemaker malfunction. Life in the Fast Lane. October 24, 2024. https://litfl.com/pacemaker-malfunction-ecg-library/.
Abu-haniyeh A, Hajouli S. Pacemaker Mediated Tachycardia. [Updated 2023 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. https://www.ncbi.nlm.nih.gov/books/NBK560831/
Refractory periods, PMT. Cardiocases. https://www.cardiocases.com/en/pacingdefibrillation/specificities/pm-av-delays-refractory-periods-management-tachycardia/medtronic#:~:text=The%20post%2Dventricular%20atrial%20refractory%20period%20(PVARP)%20is%20triggered,the%20P%20wave%20synchronous%20modes.
Authored by Michael Hohl MD and Ari Edelheit MD