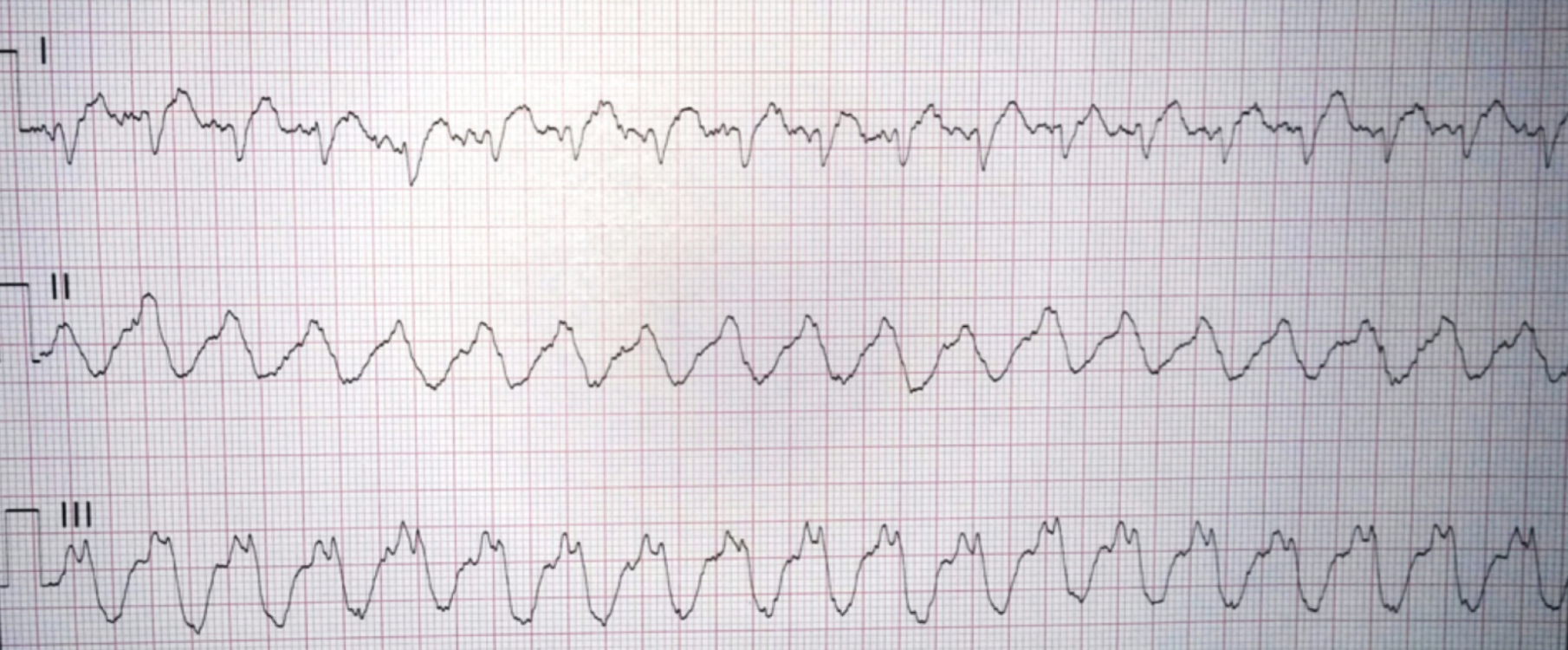
A 49-year-old male with a history of hypertension, hyperlipidemia, and a history of opioid use disorder presents to the emergency department. The tech hands you this EKG (Figure 1) and says, “Hey doc, this patient states he has palpitations, they are going to R1.”
Interpretation: Rate: 120 bpm; Rhythm: wide complex sinus tachycardia; Axis: indeterminate to left axis deviation (I: pos, II: neg, aVF: neg) Intervals: PR: 120, normal; QRS: 240, wide; QT indeterminate; P-Waves: present; QRS Complex: wide; ST Segment/T-waves: indeterminate
On initial assessment, the patient is awake and alert. He is normotensive and breathing comfortably with a normal oxygen saturation. The differential for regular wide complex tachycardias includes the following:
Ventricular tachycardia
SVT with aberrancy
SVT with bundle branch block
Antidromic AVRT
Pacemaker mediated tachycardia
Toxic metabolic syndromes
As the patient is stable, he is given 150mg of amiodarone over 10 minutes. After the amiodarone is completed, the patient appears to have a more organized rhythm on the monitor and another EKG (Figure 2) is ordered.
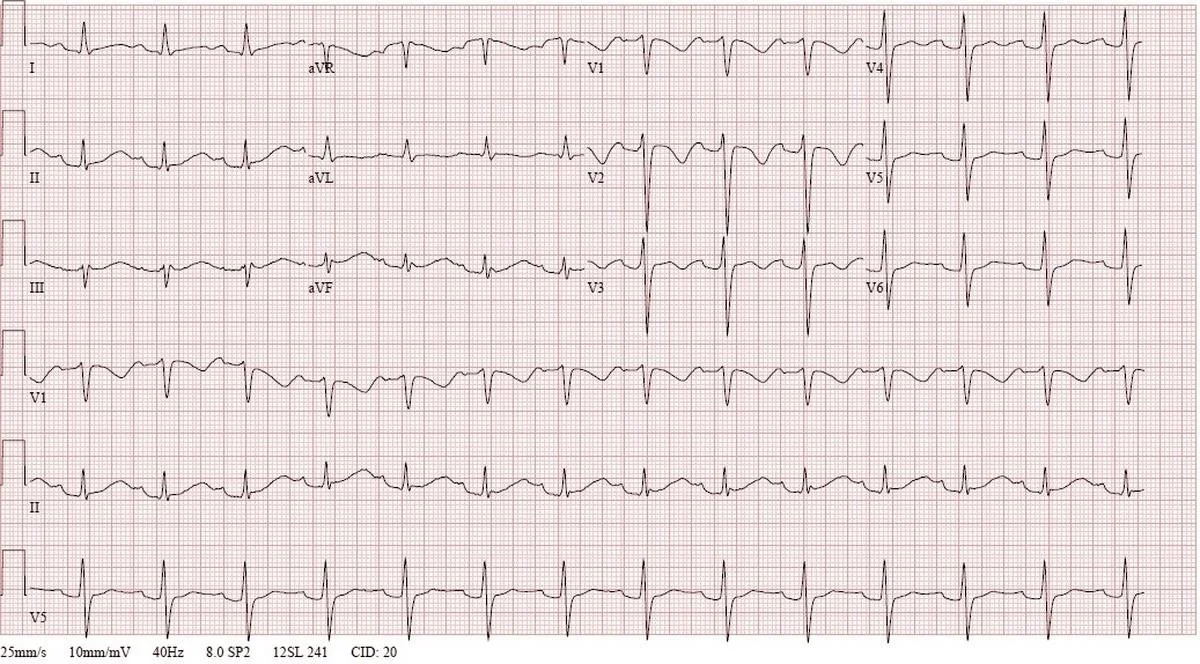
Figure 2. EKG after amiodarone administration (Image From: https://www.aliem.com/acmt-visual-pearls-drug-induced-qt-prolongation/?platform=hootsuite)
Interpretation: Rate: 84 bpm; Rhythm: sinus tachycardia; Axis: normal axis (I: pos, II: pos, aVF: neg) Intervals: PR: 200, normal; QRS: 120, normal; QTc 530, long; P-Waves: present; QRS Complex: narrow; ST Segment/T-waves: long ST segment, no ST elevations or depressions, T-wave inversions to biphasic T-waves in leads V1-V3
Despite a return to a more organized sinus rhythm, the QTc interval is now notably prolonged and your treatment approach is reformulated to reflect this new information. The differential for prolonged QTc interval is as follows:
Congenital
Electrolytes: hypokalemia, hypocalcemia, hypomagnesemia
Medications:
Antibiotics: macrolides, fluoroquinolones, bactrim
Antiarrhythmics: amiodarone, flecainide, dofetilide
Antidepressants: TCAs, venlafaxine, some SSRIs
Antiemetics: ondansetron, droperidol
Antifungals and Antimalarials
Antipsychotics
Methadone
The labs are reviewed and the patient’s electrolytes are all within normal limits. There are no prior EKGs for comparison or mentions of congenital conditions in the patient’s chart. Additional history is obtained including medications that he is taking and the patient states, “The only medication I really take is loperamide.”
Discussion
You think to yourself, “Loperamide can’t cause prolonged QTc….can it?” Well friends, I am here to tell you that yes, indeed it can! Let’s chat about loperamide toxicity and management of prolonged QTc and Torsades de Point!
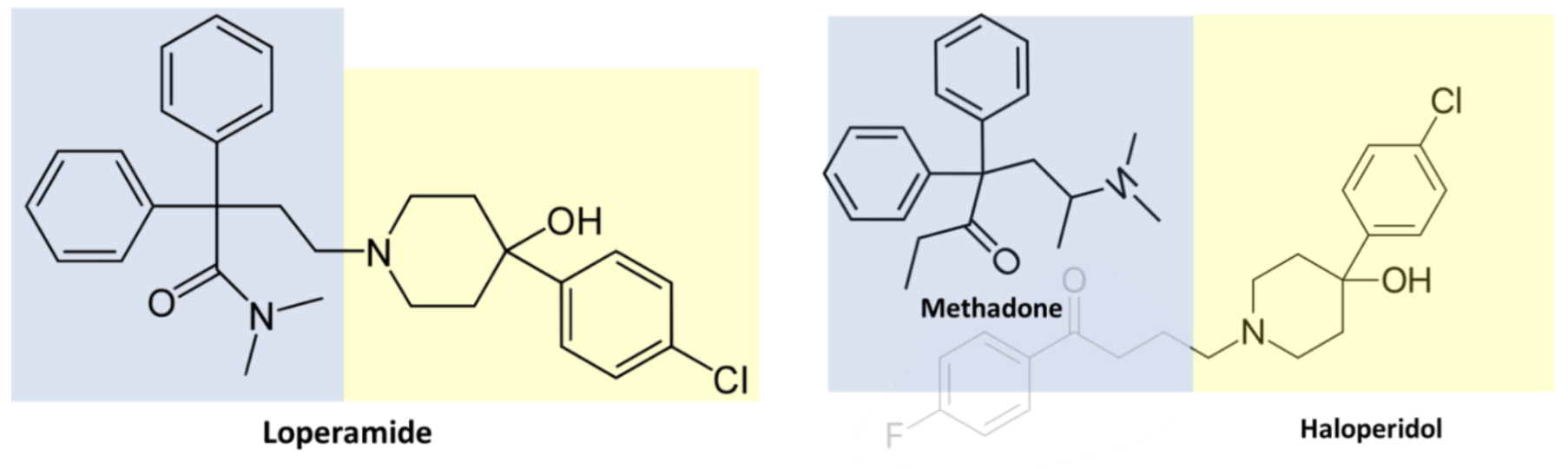
Loperamide is a medication clinically used as an antidiarrheal. However, loperamide is also used by some as a substitute for methadone or as an attempt to get the same effects one would get with opioids.
Figure 2. Structural similarity of loperamide with methadone and haloperidol (Images From: https://toxandhound.com/toxhound/worst-of-both-worlds/)
Loperamide and methadone share a very similar structure. At therapeutic doses loperamide does not cross the blood brain barrier due to the p-glycoprotein (p-gp) efflux channel. P-gp is located in the blood brain barrier, GI tract, and kidneys. Meaning that at therapeutic doses loperamide does not cause central nervous system or cardiac effects (this, however, is not true in children as they have underdeveloped p-gp). People will also take p-gp inhibitors such as cimetidine or black pepper to try to overcome P-gp so loperamide crosses the BBB.
However, in overdoses, the amount of loperamide can overwhelm P-gp and act as a mu-opioid receptor agonist causing opioid-like effects. You can even see opioid-like withdrawal in patients who chronically take high doses of loperamide and stop. At these high doses you also get blockade of the fast sodium channels and potassium efflux channels on cardiac myocytes leading to wide QRS and prolonged QTc, which can deteriorate into wide complex tachycardia as with this patient.
As always, with any wide complex tachycardia (WCT), initial treatment is focused on stabilization. In this case the initial presentation was a stable WCT and was appropriately treated with 150mg amiodarone. Alternatively, the patient could have been given the following:
6-12mg IV adenosine (carries the risk of ventricular fibrillation if presenting rhythm is not ventricular tachycardia)
50mg/min procainamide (avoid with QT prolongation!! and CHF)
100mg sotalol (avoid with QT prolongation!!)
100-200J synchronized cardioversion if unstable
Additionally, wide QTc predisposes patients to torsades de point (TdP). Had one of the QT prolonging agents above been chosen, or the patient did not respond to initial treatments, it is very likely the presenting monomorphic VT or sinus rhythm with prolonged QTc could have progressed to polymorphic VT or TdP. Mainstays for treatment of TdP include the following:
2g loading dose IV Magnesium Sulfate followed by 1-4g/hr infusion
5mcg/min Isoproterinol (goal 30 bpm higher than native heart rate)
Overdrive pacing (goal 30 bpm higher than native heart rate)
100-200J defibrillation if unstable
Take Home Points
Stable wide complex tachycardias get medications, unstable wide complex tachycardias get electricity
Loperamide is an antidiarrheal that can be abused and at high doses acts as a mu-opioid receptor agonist causing opioid-like effects
Traditional antiarrhythmics may be ineffective or carry side effects that may worsen the clinical condition
Consider toxic metabolic syndromes, including overdoses and abuse when you see a dysrhythmia is the ED. “It’s always tox!” – Dr. Sean Bryant
References
Marraffa J. Tox and Hound – The Worst of Both Worlds. The Tox and the Hound. November 26, 2018. Available at: https://toxandhound.com/toxhound/worst-of-both-worlds/.
Nelson LS, Olsen D. Opioids. In: Nelson LS, Howland M, Lewin NA, Smith SW, Goldfrank LR, Hoffman RS. eds. Goldfrank's Toxicologic Emergencies, 11e. McGraw-Hill Education; 2019.
Marino R, Pizon A. ACMT toxicology visual pearls: Drug-induced qt prolongation. ALiEM. Available at: https://www.aliem.com/acmt-visual-pearls-drug-induced-qt-prolongation/.
Morgenstern J. Torsades de Pointes: Approach to resuscitation. First10EM. December 15, 2023. Accessed December 30, 2025. https://first10em.com/torsades-de-pointes/.
Authored by Taylor Wahrenbrock MD, Michael Hohl MD, and Ari Edelheit MD