The Case:
The patient is a 53-year-old man with a history of none who presented to the emergency department with an atraumatic painful and red left big toe for 3 days. The onset was slow and gradual, and limited to the left big toe. He had never had pain or redness like this before in his toes. He denied any trauma to the joint. No significant or debilitating pain with moving the joint, however mild pain noted. He denied fever or chills, open wounds.
The patient had no known history of gout, though did endorse eating meat and chicken liver. Denied history of diabetes. Denied history of allergies to any medications.
On exam, there was swelling and erythema at the base of the first great toe on the left foot. The patient had moderate pain on passive and active range of motion of the joint. There were no other findings of examination of all other joints in the lower extremities.
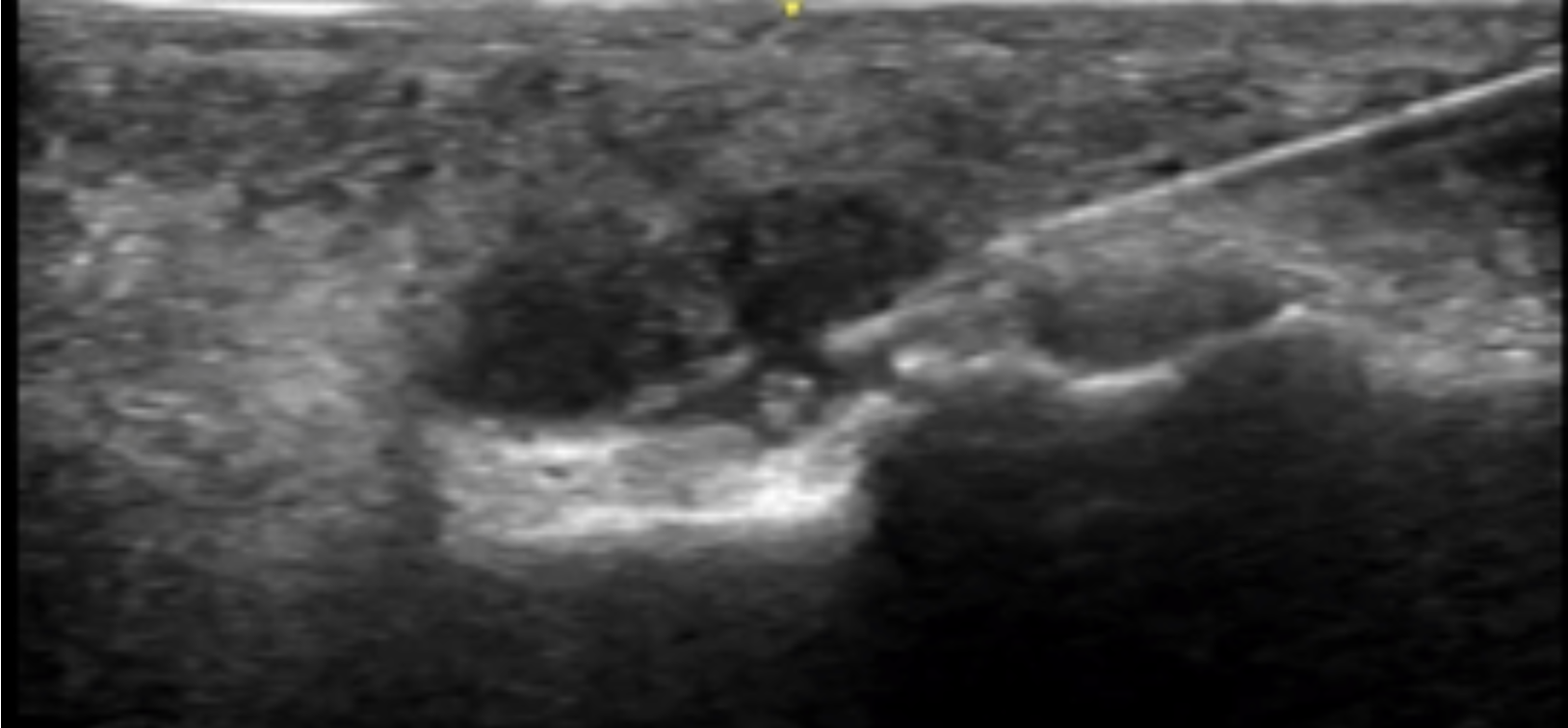
On point-of-care ultrasound (POCUS), a small joint effusion on the affected left big toe is seen with a maximum diameter of about 5mm.
The differential was most concerning for septic joint versus gout given the physical examination with erythema, pain with range of motion, and the presence of a joint effusion on POCUS.
An ultrasound guided arthrocentesis was performed using in-line needle visualization technique.
About 1.5cc fluid was obtained. The arthrocentesis yielded findings of monosodium urate crystals, negative Gram staining, only 372 WBC. Gout was diagnosed. The patient was discharged with naproxen and a prednisone taper. Instructions regarding lifestyle changes related to reducing risk of future gout attacks discussed.
Discussion:
Ultrasound as a tool is highly effective in detecting joint fluid given its high sensitivity (Draghi et al), lack of radiation, cost effectiveness, and its use in rapid bedside assessment. To do so — use a linear probe to find the joint in the long axis and identify the hypoechoic fluid in relation to the joint space. Scan both in long and short axes to fully characterize the effusion. When performing a musculoskeletal ultrasound, you should always examine the affected joint as well as the contralateral unaffected side for comparison.
Once the effusion is noted, a decision must be made regarding if arthrocentesis for diagnostic or therapeutic reasons is needed. In our case, a diagnostic arthrocentesis was needed as direct fluid analysis is the gold standard in this case to rule out septic arthritis.
When there is an effusion present in the large joints such as the knee, the size can range from 10mL up to even 30mL of fluid – making a landmark guided arthrocentesis feasible given the large target of fluid. However medium-sized joints such as the ankle or elbow often hold much less synovial fluid for sampling. Even smaller joints, such as the metatarsophalangeal joint can hold even smaller amounts, making successful arthrocentesis difficult. An unsuccessful tap can lead to consultation of subspecialties, unnecessary hospitalization, and a lack of data to help guide the patient’s course.
A recent randomized clinical trial (Gibbons et al) was performed in 2022 to answer the question as to if ultrasound guided arthrocentesis was superior to landmark guided arthrocentesis in medium-sized joints (elbow, wrist, ankle). It was a prospective, single center study that included all adults who required arthrocentesis of a medium sized joint and excluded those who were unable to consent, those who had a prosthetic joint, those who had an overlying infection, and those who were on anticoagulation. The patients were randomized to either ultrasound or landmark guided arthrocentesis and an EM resident performed the procedure. The number of attempts, complications (hematoma, hemarthrosis, infection, neurovascular injury), and first-pass success was analyzed.
For overall success, the ultrasound guided group was 94.1% successful, and the landmark guided group was 60% successful - difference 34.1% (CI 4.9-58.83). Note that some patients who were initially in the landmark guided group were crossed over to the ultrasound guided group if there were three unsuccessful attempts made. Eight patients in the landmark guided group were found to have no effusion at all after cross-over to the ultrasound group. With an intention to treat analysis – the overall success for the ultrasound guided group was 85% and the landmark guided group was 39.1% – difference 46% (CI 16.91-65.56). In regards to first pass success, the ultrasound guided group had a 82.4% first pass success rate and the landmark guided group had a 46.7% first pass success rate – difference 35.7% (CI 2.76- 60.37). There were 1.35 mean attempts in the ultrasound guided group and 2.00 in the landmark guided group – Difference 0.65 (CI 0.005 - 1.295). There were no complications in either group.
While this study suffers from a few limitations (did not specify effusion size of patients in relation to success/failure of arthrocentesis attempt, groups not completely matched in regards to the presence of effusion as there were less effusions ultimately in the landmark based group, amongst others), it demonstrates that ultrasound can improve both overall success rate and first pass success – reducing pain for the patient, increasing yield of fluid. There are other studies also supporting the utility in using ultrasound for procedural guidance with arthrocentesis – Sibbit et al demonstrated that it can reduce procedural pain, increase the synovial fluid yield, and can improve therapeutic outcomes at two weeks.
In our case, we were dealing with an effusion that measured 0.5cm by 2cm at its largest dimensions – it was a tiny effusion. Without the use of ultrasound, obtaining fluid from this tiny pocket would have been very difficult. The patient’s MTP was prepped using sterile procedure and an ultrasound probe cover was utilized to ensure sterility. We used in-line technique, as demonstrated in the above video.
Ultimately, we were successful in obtaining a small amount of fluid for analysis which supported the diagnosis of gout and the patient was able to be safely discharged with a treatment plan and follow up. Consider using ultrasound both to identify the effusion in your next patient with joint pain – and also, in the arthrocentesis itself.
Thank you to UltrasoundGel for their comprehensive analysis of Gibbons et al.
References:
Draghi F, Urciuoli L, Alessandrino F, Corti R, Scudeller L, Grassi R. Joint effusion of the knee: potentialities and limitations of ultrasonography. J Ultrasound. 2015 Sep 18;18(4):361-71. doi: 10.1007/s40477-015-0180-3. PMID: 26550074; PMCID: PMC4630268.
Sibbitt WL Jr, Kettwich LG, Band PA, Chavez-Chiang NR, DeLea SL, Haseler LJ, Bankhurst AD. Does ultrasound guidance improve the outcomes of arthrocentesis and corticosteroid injection of the knee? Scand J Rheumatol. 2012 Feb;41(1):66-72. doi: 10.3109/03009742.2011.599071. Epub 2011 Nov 21. PMID: 22103390.
Gibbons RC, Zanaboni A, Genninger J, Costantino TG. Ultrasound-versus landmark-guided medium-sized joint arthrocentesis: A randomized clinical trial. Acad Emerg Med. 2022 Feb;29(2):159-163. doi: 10.1111/acem.14396. Epub 2021 Oct 23. PMID: 34608713.
Michael Prats. US-Guided Arthrocentesis: A Randomized Clinical Trial. Ultrasound G.E.L. Podcast Blog. Published on April 25, 2022. Accessed on August 12, 2025. Available at https://www.ultrasoundgel.org/124.
Authored by Dr. Priyanka Pradhan and Dr. Dave Murray