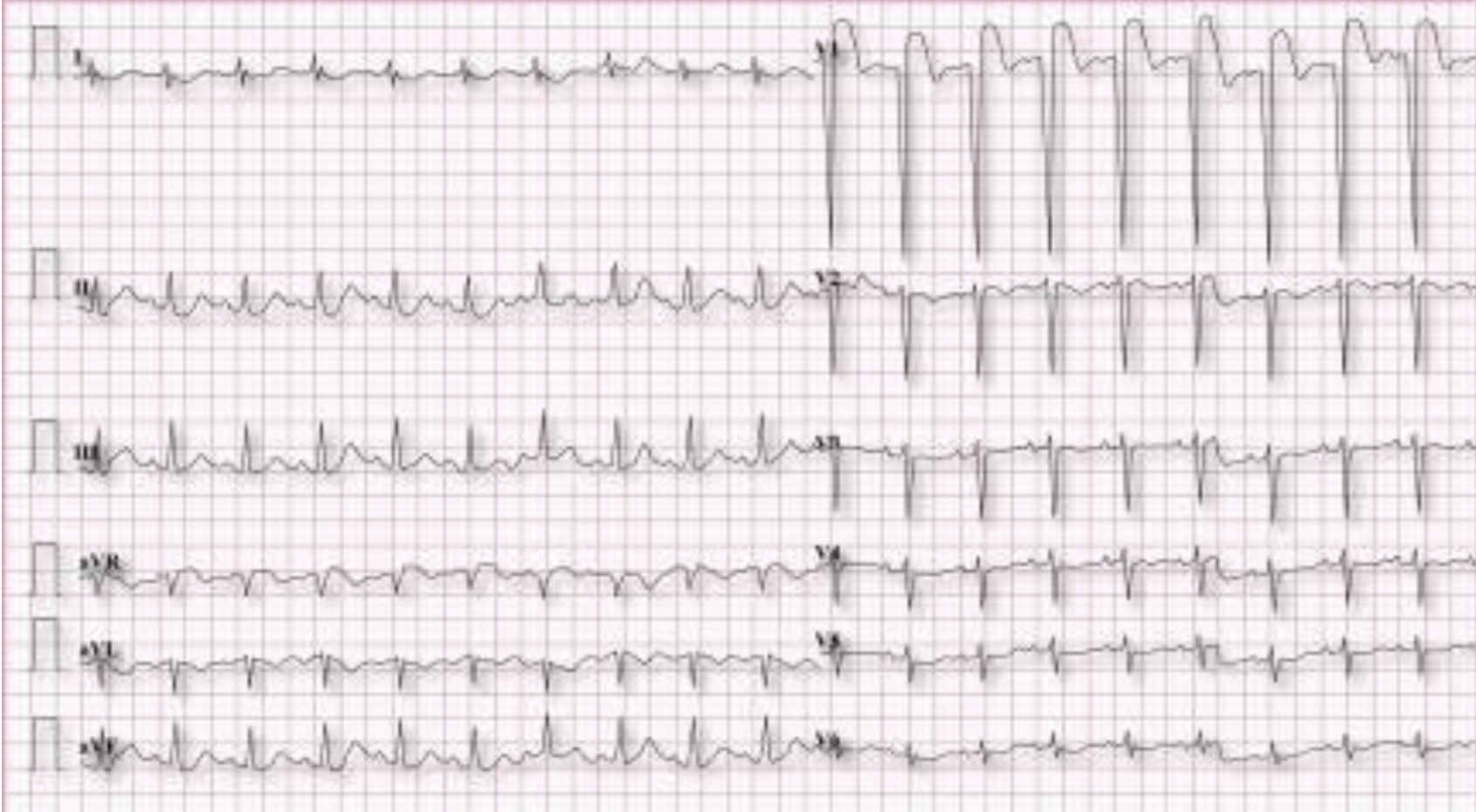
The patient is a 46 year old female who is presenting for concern of epigastric pain, nausea and vomiting. The patient has a history of chronic nausea, bipolar disorder, diabetes on insulin, and gastroparesis. Given her age and chief complaint, an EKG (Figure 1) was ordered to rule out atypical ACS.
Interpretation: Rate: 70 bpm; Rhythm: regular; Axis: extreme right axis deviation (I: neg., II: neg., aVF: neg) Intervals: PR: 150, normal; QRS: 75, normal; QT: 490, mild prolongation; P-Waves: inverted in I, aVL, V1; QRS Complex: poor R wave progression; ST Segment/T-waves: inverted T waves in I, II, aVL, V1
When evaluating this EKG, the computer analysis reads “Limb lead reversal.” However, upon reviewing the rest of the patient chart, each of her EKGs is consistent with this morphology.
What is the diagnosis? What findings on EKG can help us determine this?
The diagnosis for this patient can be easily seen on CXR (in Figure 2 below). She has a history of situs inversus with dextrocardia, which is what causes the EKG changes above.
Because the EKG leads are traditionally placed over the left chest, when patients have inverted anatomy, the vectors of electricity travel differently through the heart, causing these distinctive EKG changes:
Absent R wave progression in the pre-cordial leads
Negative P, QRS, and T in Lead I
Positive P, QRS, and T in aVR
Marked right axis deviation
If these EKG changes are present, the first step you should take is ensuring that the EKG leads are all placed appropriately, particularly the arm leads. Reversal of the left and right arm leads will show a similar right axis deviation with an inverted P wave in lead I. This is far more common than dextrocardia itself. After confirming correct lead placement, CXR or bedside echo can help further elucidate this diagnosis.
Figure 2. Patient XR Chest
How should you modify the EKG lead placement?
To obtain a “normal” EKG in a patient with dextrocardia, you need to reverse BOTH the arm leads and the chest leads. Figure 3 below shows an example of appropriate lead placement in a patient with confirmed dextrocardia.
Figure 3. EKG leads for dextrocardia (Image adapted from: https://litfl.com/ecg-lead-positioning/)
Do you really need to change the lead placement? Won’t you still see an MI?
Since dextrocardia is such a rare occurrence, the case reports on acute myocardial infarction and other acute cardiac disease in these patients are sparse. However, it is recommended that you ALWAYS obtain reversed leads in these patients as an acute MI can be more difficult to diagnose when only looking at the traditional left-sided leads. In multiple case reports, acute anterior MI only presents with V1 or aVR ST segment elevation in the left-sided leads, but upon obtaining reversed leads, it becomes clear there is far more expansive disease. This can lead the provider to either miss this diagnosis altogether or to believe that a patient has a less significant defect, and not understand the true extent of disease.
The figures below are from a case report showing this phenomenon, with left-sided leads in Figure 4 and right-sided leads in Figure 5.
Figure 4: Left sided EKG in dextrocardia showing ST segment elevation V1 (Image obtained from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8312012/)
Figure 5: Right sided EKG obtained from same patient showing evidence of extensive anterior MI with elevations in leads V2-V5. (Image obtained from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8312012/)
What about posterior leads?
As one can imagine, the occurrence of posterior STEMI in dextrocardia is an even more rare occurrence, and there is little guidance in formal literature about diagnosis and EKG technique. However, there is a case report describing a left circumflex occlusion MI in dextrocardia that outlines the importance of proper lead placement of V7-V9 to appropriately diagnose posterior MI. In this case report, by Huang et. al., a patient with dextrocardia was incorrectly diagnosed with an NSTEMI. Later on, a posterior lead EKG, in which leads V7-V9 were placed on the right in the mirror image of traditional left-sided posterior leads, was obtained and showed diffuse ST segment elevation.
Are patients with dextrocardia more at risk for heart disease? Should I raise my clinical suspicion for ACS?
Dextrocardia alone does not pose a heightened cardiac risk. However, some patients may have dextrocardia in conjunction with other congenital anomalies, which could increase risk in these individuals. It is important to take a thorough medical and surgical history in these patients to assess for other co-existing cormorbidities.
Take-away Points:
If your EKG is looking suspicious, a good first step is to always ensure proper lead placement to assess for user error
When suspecting dextrocardia, look for these specific EKG changes to confirm: primarily negative deflection in I with an inverted P wave, positive deflection in aVR, poor R wave progression and right axis deviation.
In dextrocardia patients, a traditional left-sided EKG is not good enough to rule out MI. ALWAYS take the extra time to obtain an EKG with mirrored right sided lead placement to appropriately evaluate for signs of ischemia.
Dextrocardia itself can be asymptomatic, however you should be wary of coexisting conditions that may increase cardiac risk.
References:
Nickson, C. Buttner, R. Dextrocardia. Life in the Fast Lane. July 19, 2021. https://litfl.com/dextrocardia-ecg-library/
Mozayan C, Levis JT. ECG Diagnosis: Dextrocardia. Perm J. 2019;23:18-244. doi: 10.7812/TPP/18.244. Epub 2019 Aug 15. PMID: 31496498; PMCID: PMC6730946.
Cadogen, M. ECG Lead Positioning. Life in the Fast Lane. Jan. 30, 2022. https://litfl.com/ecg-lead-positioning/
Winter JL. Recognition of Anterior STEMI in Dextrocardia and the Importance of Right-Sided Chest Leads. JACC Case Rep. 2020 Jul 15;2(8):1222-1226. doi: 10.1016/j.jaccas.2020.06.009. PMID: 34317454; PMCID: PMC8312012.
Huang Y, Zhou H, Wu L. Acute total occlusion of left circumflex artery in a patient with dextrocardia and situs inversus. Journal of International Medical Research. 2020;48(1). doi:10.1177/0300060519893180
Authored by Erica Dolph MD and Ari Edelheit