Recommended Citation: Frendo S, Roussas A. The Heart Of The Matter - A Case Of Recurrent Chest Pain [Internet]. Cook County Emergency Medicine Residency;Available from: https://cookcountyem.com/blog/2024/4/24/the-heart-of-the-matter-a-case-of-recurrent-chest-pain
The Case:
A 50-year-old male with a history of tobacco use disorder presents with 1 week of intermittent, central, pressure-like chest pain that lasts a few minutes at a time without clear exacerbating or relieving factors. He had a particularly severe episode just before arrival but is now pain free. The initial ECG is shown in Figure 1. A serum troponin was negative. The patient leaves against medical advice but returns two days later with persistent symptoms. A second ECG is shown in Figure 2. An initial serum troponin is 0.048 ng/mL and uptrends to a maximum 1.792 ng/mL. His vital signs on both visits are within normal limits.
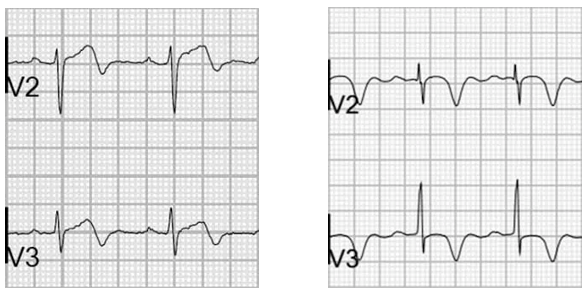
Figure 2. ECG from 2nd visit notable for inverted T waves in lead V2 and biphasic T waves in leads V3 and V4.
Interpretation:
The patient’s first ECG (Figure 1) was notable for normal sinus rhythm, normal rate, axis, and intervals. Of note, slight ST depression, borderline biphasic T-waves in V2, and borderline ST elevation in III.
The patient’s second ECG (Figure 2) was notable for normal sinus rhythm, normal rate, axis, and intervals. Of note are prominent inverted T waves in V2 and biphasic T waves in V3/V4.
Discussion:
Figure 3. Example ECG’s displaying Type A Wellens’ syndrome (left) and Type B Wellens’ syndrome (right) courtesy of https://litfl.com/wellens-syndrome-ecg-library/.
These ECG findings are consistent with Type B Wellens’ syndrome, which is a STEMI equivalent. Type A (25% of cases) Wellens’ syndrome is comprised of biphasic T waves with an initial upward deflection in precordial leads (most prominent in V2 and V3, but can be found in any of the precordial leads) and Type B (75% of cases) Wellens’ syndrome is comprised of deeply and symmetrically inverted T waves in anterolateral leads (1), seen in Figure 3. Of note, the syndrome is excluded if precordial leads are notable for ST elevation, Q waves, or loss of R wave progression (2). This is a spectrum of disease, and often Type A waves will convert into Type B waves, as seen in Figure 4. These ECG findings are typically present when a patient is pain-free and persists for days to weeks.
Figure 4. Progression of Wellens syndrome from Type A to Type B pattern courtesy of https://litfl.com/wellens-syndrome-ecg-library/.
Though there are many theories, Wellens is thought to most likely arise from intermittent occlusion of a critically stenotic LAD with subsequent thrombus lysis. Patients will present with only small troponin elevation or may be entirely normal (2-4). Of note, up to 75% of patients will have an anterior wall MI within one week without intervention (5). Initial treatment typically involves aspirin load and is followed by antiplatelets, heparin, beta-blockers, and/or nitrates in conjunction with cardiology consultation. Management of this syndrome should involve the following precautions:
Precautions:
Even with a normal troponin, this EKG should initiate a cardiology consult for expedited PCI (within 24 hours) as the patient is at high risk of MI—medical management alone is insufficient (2-4).
These patients should NOT undergo stress testing, as this can cause further ischemic damage (2-4).
Beware of pseudo-normalization of the T waves. If the patient has recurrent chest pain, and the T waves are now upright, initiate a discussion with cardiology as they are likely an evolving STEMI (2-4).
Cannot be applied to patients with LVH (4).
Although Wellens is commonly thought of as a STEMI equivalent, the 2022 ACC Expert Consensus Decision Pathway instead categorizes it as an ischemic change (6). Keep this in mind when discussing with your consultants.
Case Conclusion:
Figure 5. Coronary angiography before and placement of a drug-eluting stent.
The patient underwent LHC and was found to have a 95% proximal stenosis of the LAD. The patient underwent PCI and a DES was placed with no complications, with the resultant PCI seen in Figure 5. The patient was discharged after 48 hours of observation with no further episodes of chest pain. He was started on aspirin, clopidogrel, high-dose statin, and metoprolol. At cardiology follow-up four months later, he is doing well without recurrence of symptoms or evidence of heart failure.
Authored by Samson Frendo, MD and Adam Roussas, MD.
References:
Rhinehardt J, Brady WJ, Perron AD, Mattu A. Electrocardiographic manifestations of Wellens' syndrome. Am J Emerg Med. 2002;20(7):638-643. doi:10.1053/ajem.2002.34800
Cadogan M, Buttner R. Wellens Syndrome [Internet]. Life in the Fast Lane • LITFL. 2020 [cited 2024 Apr 23];Available from: https://litfl.com/wellens-syndrome-ecg-library/
Miner B, Grigg WS, Hart EH. Wellens Syndrome. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482490/
Mead NE, O'Keefe KP. Wellen's syndrome: An ominous EKG pattern. J Emerg Trauma Shock. 2009;2(3):206-208. doi:10.4103/0974-2700.55347
de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103(4 Pt 2):730-736. doi:10.1016/0002-8703(82)90480-x
Writing Committee, Kontos MC, de Lemos JA, et al. 2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain in the Emergency Department: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022;80(20):1925-1960. doi:10.1016/j.jacc.2022.08.750