The Case:
A 58-year-old male with no reported past medical history presents with central chest “irritation” and exertional dyspnea for 1 day. He his hypotensive and diaphoretic upon evaluation. An initial ECG followed by a right sided ECG is obtained (Figures 1 and 2).
Interpretation:
Rate: 65 bpm; Rhythm: regular; Axis: normal (I+, II+ aVF+); Intervals: PR 176, QRS 106, QTc 408; P-Waves: present preceding each QRS; QRS complex: narrow, Q-waves in V1-V3; ST Segment/T-waves: STE in III (1.3mm) and aVF (~0.9mm, wandering baseline) with reciprocal STD in 1, aVL (down sloping) and V2, V3 (horizontal). Horizontal STD also in V4 (2mm), V5 (1mm), V6 (1mm). Prominent anterior T-waves.
A right sided ECG was promptly obtained.
Figure 2. Repeat ECG with right-sided leads obtained ten minutes after index ECG.
Interpretation:
Rate: 78 bpm; Rhythm: regular; Axis: normal (I+, II+ aVF+); Intervals: PR 180, QRS 110, QTc 396; P-Waves: present preceding each QRS; QRS complex: narrow, Q-waves in V1-V3, and now V4-V6; ST Segment/T-waves: Progressive STE in III (1.8mm) and aVF (~1.5mm, wandering baseline) with deepening reciprocal STD in 1, aVL (down sloping) and V2R (horizontal). V3R isoelectric. V4R-6R isoelectric vs very slight (0.1-0.5mm) convex STE.
Questions to consider:
What primary lesion(s) does this patient likely have?
How can one utilize the dynamic electrical features of this ECG to help localize lesions?
What does the presence of q-waves indicate on this ECG?
Discussion:
First, it’s important to remember the universal definition of a STEMI (Sandoval). A summary table has been provided in Appendix A below.
The initial ECG shows STE elevation >1 mm in III and questionable STE with ST segment flattening aVF with reciprocal STD in aVL and lead I. Although the lead II ST segment is isoelectric, these changes are concerning for an inferior myocardial infarction (IMI). Approximately 80% of inferior STEMIs are caused by a dominant right coronary artery, though 18% of cases can arise from a dominant left circumflex (LCx) (Warner). Lead I can help differentiate the two: if there is reciprocal STD in lead I, then there is likely an RCA occlusion. RCA occlusion is further suggested by STE in lead III > II and STE in V1 and V4R (Appendix A, Figure 1) (Buttner). This is because the RCA perfuses the medial territory of the inferior and septal portions of the inferior wall, which are down and rightward projecting electrical vectors, therefore resulting in a more pronounced STE in lead III (rightward vector) than lead II (leftward vector) (Appendix A, Figure 4). To the contrary, in the absence of STD in lead I, a circumflex lesion is more likely and further suggested by STE in lead II = III and STE in the lateral leads (I, aVL, V5-6). This is because the LCx perfuses the lateral and left posterobasal territory of the inferior wall, resulting in an ischemic vector directed inferiorly and leftward. Although uncommon, the left anterior descending (LAD) can also be the culprit in an IMI. These are called “type III’ or “wrap around” lesions and are defined by a pattern of inferior and anterior STE. Therefore, evaluation of our patient’s inferior, high lateral, and right-sided leads is suggestive of an acute RCA occlusion.
Once an IMI has been identified, the next clinical question is if there is a right ventricular myocardial infarct (RVMI). On a traditional 12-lead ECG, the most specific ECG finding is STE in V1 and STD in V2. Other findings include STE in V1, isoelectric ST segment in V1 with marked STD in V2, and STE III > II (Nagam). The diagnosis is made by performing a right-sided ECG (Appendix A, Table 1) and finding any STE in V3R-V6R. An STE of >1.0mm in V4R is diagnostic (Nagam). In the case of our patient, we see a Q-wave in V1 with an isoelectric ST-segment, deep STD depression in V2, and STE III > II which is highly suggestive of a right-sided lesion. Right-sided leads were pursued, and while not showing explicit STE, there is significant change in morphology with complete obliteration of the R-waves and convex upward# ST-segment that appears to be reaching towards STE in V3R-V6R. All these findings are suggestive of a right ventricular myocardial infarction.
Prompt identification of an RVMI is critical, as reduced right ventricular ejection fraction is associated with major complications including high-grade atrioventricular block, ventricular arrhythmia, and a 2.6-fold increase in mortality risk (Hamom). Further, RVMI causes significant mechanical disruption of the heart. RV failure results in elevated right ventricular (RV) volume and end-diastolic pressure, displacing the septum towards a now volume depleted RV, initiating a vicious spiral of limited ventricular filling and decreased cardiac output (Farkas). These patients are preload dependent. Thus, pre-load reducing agents (diuretics, beta-adrenergic blockers, morphine, and nitrates*) should be avoided, and hemodynamic instability should be addressed first with intravenous fluid resuscitation. If necessary, a low threshold should be maintained to initiate inotropic support (e.g. dobutamine, norepinephrine).
We have convincingly determined there is likely an RCA lesion causing IMI with RV extension, but might there be any other lesions? Namely, why does this patient have deep anterior Q-waves? Q-waves can be physiologic or pathologic. Physiologic Q-waves are typically small, but deep (>2mm) in leads III and aVR are normal variants. Q-waves are considered pathologic if present in leads V1-V3, >40ms wide, >2mm deep, and/or 25% of the depth of the QRS complex. Pathologic Q-waves indicate a current or prior myocardial infarction, hypertrophic cardiomyopathy, infiltrative myocardial disease, or lead placement errors (e.g., upper limb lead placed on the lower limb leads) (Burns). For our patient, these Q-waves are abnormal and suggestive of either acute or previous disruption in blood supply to the anterior septal wall, which is provided by the LAD and branches of the LCx. Therefore, these findings are concerning for multi-vessel disease. The T-waves appear large relative to the absent R-wave and may represent hyperacute T-waves suggestive of acute ischemia. The deep horizontal ST depressions are also suggestive of possible posterior involvement. While the R/S ratio is <1 in V2, posterior leads were not obtained.
# Upward convexity or horizontal ST-segment morphologies are extremely important to recognize, as they raise the pre-test probability of cardiac ischemia in electrical tracings that may not appear to represent ischemia by traditional definitions (Mattu).
* Although it is traditionally taught to avoid nitrates in RVMI, the foundational data supporting this practice is weak. Newer, more robust literature suggests there is little-to-no harm patients with RVMI who receive nitrates and a potential benefit of analgesic and thus sympathetic control in these patients (Rezaie).
Case Summary and Resolution:
The IMI/RVMI pattern was quickly identified by the emergency medicine physicians. The cath lab was activated. The patient’s hypotension was improved with a 500cc bolus of IVF, and pain was controlled with aspirin. PCI showed a 90% distal RCA occlusion, 95-99% obtuse marginal occlusion, and 99% chronic total occlusion of the LAD. Given triple vessel disease, cardiothoracic surgery was consulted intraoperatively, and a coronary artery bypass grafting (CABG) procedure was performed. The patient was also found to be in cardiogenic shock and required hemodynamic support with an intra-aortic balloon pump for several ICU days.
This patient’s presenting ECG demonstrated STE in III and aVF with reciprocal STD in I and aVL suggestive of an inferior myocardial infarction secondary to RCA occlusion. RVMI was suggested by an isoelectric ST segment in V1 and deep horizontal STD in V2, and then highly suggested by right-sided leads showing R-wave obliteration and inversion of STD in V3R-V6R and convex ST segment morphology in V4R. The ECG also showed Q-waves in the anterior leads suggestive of coexisting LAD or distal LCx/Obtuse marginal disease.
Take Away Points:
Inferior STEMI
STE >1.0mm in II, III, aVF with reciprocal STD in aVL
RCA suggested by STD in Lead I and STE III>II
LCx suggested by normal Lead I and STE III = II
Type III or “wrap around” STEMI suggested by coexisting anterior lead STE
Right ventricular infarct
Consider in all IMI
STE in V1 and STD in V2 (most specific)
Isoelectric ST-segment in V1 with STD in V2
STE III > II
Right-sided ECG shows STE in V3R-V4R
STE in V4R > 1.0 mm (diagnostic)
Morbidity and Mortality
High-grade atrioventricular block and ventricular arrhythmias
Preload dependent
2.6x increase in mortality
Vicious spiral
RV insufficiency and dilation = elevated RV pressures and decreased RV output = bowing into LV = diastolic LV failure = decreased cardiac output = cycles on self via more physiology
Manage with fluids and inotropes
Q-waves
Always pathologic in anterior leads
Suggestive of acute or chronic ischemia
Appendix A:
Table 1. Universal definition of ST-Elevation Myocardial Infarction (Sandoval). Of note, there are numerous STEMI-equivalents, as well as the burgeoning OMI/NOMI paradigm to also consider, though these are beyond the scope of this review.
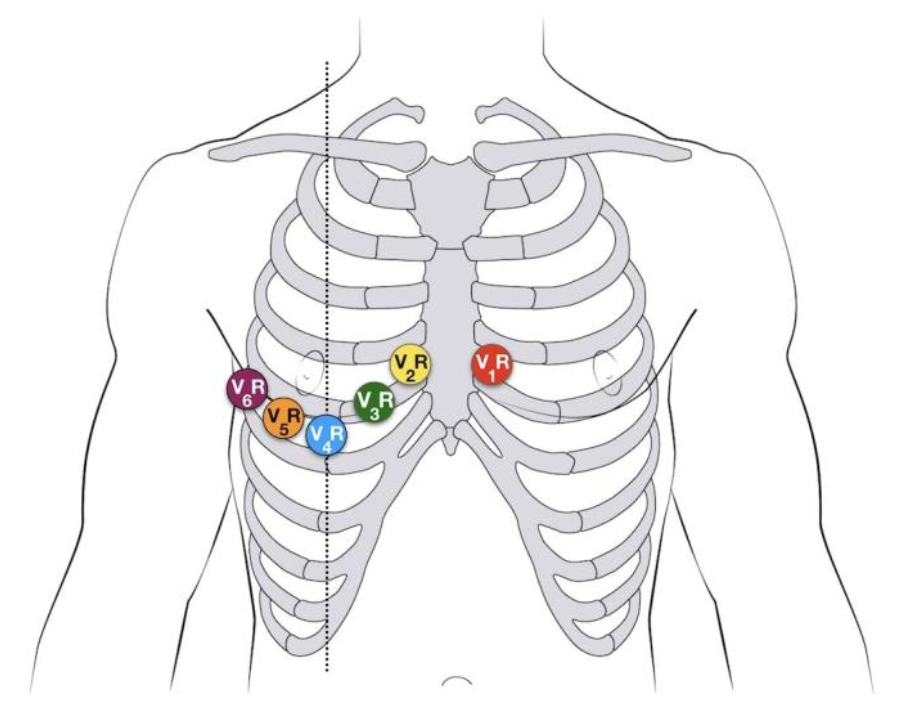
Figure 3. Right-sided ECG lead placement. Courtesy of LIFTL (Buttner).
Figure 4. Electrode visual axes. Courtesy of CardioSecure.
Authored by Adam Roussas, MD.
References:
Burns, E., & Buttner, R. (2020, August 1). Q wave • LITFL • ECG library basics. Life in the Fast Lane • LITFL. https://litfl.com/q-wave-ecg-library/
Buttner, R., & Burns, E. (2018, August 1). Inferior STEMI • LITFL • ECG library diagnosis. Life in the Fast Lane • LITFL. https://litfl.com/inferior-stemi-ecg-library/
Farkas, A. Emc. (2024, August 21). Right Ventricular failure. EMCrit Project. https://emcrit.org/ibcc/rv/#pathophysiology_of_RV_failure
Hamon, M., Agostini, D., Le Page, O., Riddell, J. W., & Hamon, M. (2008). Prognostic impact of right ventricular involvement in patients with acute myocardial infarction: Meta-analysis. Critical Care Medicine, 36(7), 2023–2033. https://doi.org/10.1097/CCM.0b013e31817d213d
Mattu, A. (n.d.). UMEM educational pearls. University of Maryland School of Medicine, Department of Emergency Medicine. Retrieved September 2, 2024, from https://umem.org/educational_pearls/?author=107&page=5
Nagam, M. R., Vinson, D. R., & Levis, J. T. (2017). ECG diagnosis: Right ventricular myocardial infarction. The Permanente Journal, 21, 16–105. https://doi.org/10.7812/TPP/16-105
Rezaie, S. (2024, March 18). REBEL cast ep124: Nitrates in right sided mis? REBEL EM - Emergency Medicine Blog. https://rebelem.com/rebel-cast-ep124-nitrates-in-right-sided-mis/
Sandoval, Y. (2020). The universal definition of myocardial infarction. Circulation.
Warner, M. J., & Tivakaran, V. S. (2023). Inferior myocardial infarction. StatPearls.