The Case: A 56-year-old man with diabetes, gout, and cirrhosis presented to the ED for evaluation of lower back pain localized to the midline lumbar spine for the last 3-4 months. He had previously been evaluated at two other hospitals and diagnosed with osteomyelitis/discitis. He had been treated twice with IV vancomycin for a total of ten weeks of treatment. He denied any fever, saddle anesthesia, numbness, tingling, urinary/bowel incontinence, or history of IVDU. Additionally, 3 days prior to presentation to the ED, he developed a tender mass on his left chest with pain radiating into the left shoulder. Additional ROS was significant for fatigue and chills, but otherwise was negative.
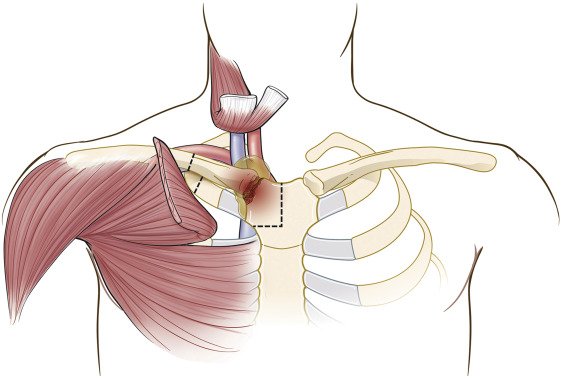
Examination was significant for an erythematous, tender nodule over the left sternoclavicular joint and moderate L2-L4 midline tenderness. His neurologic exam was normal, although back range of motion was limited secondary to pain. His vitals were all within normal limits. Lab work demonstrated significant leukocytosis (25.3) and elevated CRP and ESR. Given the finding overlying the sternoclavicular joint, there was concern for septic arthritis secondary to ongoing lumbar osteomyelitis/discitis. Chest CT confirmed a left sternoclavicular joint soft tissue lesion extending into the anterior mediastinum concerning for septic arthritis.
Orthopedics and cardiothoracic surgery were consulted in the ED. He was treated with ceftriaxone and vancomycin and admitted to medicine for further management. On hospital day 2, the patient was taken to the OR with orthopedics and CT surgery for medial clavicle resection and debridement of the sternoclavicular joint, manubrium, and necrotic mediastinal tissue. Blood and intra-operative cultures grew MRSA. He was treated with daptomycin and discharged 14 days later to a skilled nursing facility with a PICC line to complete 6 weeks of antibiotic treatment.
Why it matters: Septic arthritis is a “don’t miss” diagnosis in the emergency department, and an acutely swollen, tender joint with restricted range of motion is septic arthritis until proven otherwise (1). Unfortunately, there is no specific clinical presentation or laboratory value that definitively confirms the diagnosis. Some of the most common symptoms include joint swelling (85%) and fever (57%), but absence of these symptoms does not exclude the diagnosis (1). Large joints (knee, shoulder, hip, ankle, elbow, etc) are more commonly affected, but septic arthritis can also be seen in smaller joints (2). Hematogenous spread is the most common source of septic arthritis, but it can also be caused by direct inoculation or rarely by extension of an overlying soft tissue infection into the joint (2). If the diagnosis is suspected, orthopedic consultation is indicated for possible joint irrigation and the patient should be empirically treated with antibiotics that cover for staphylococcus and streptococcus (generally vancomycin plus a third generation cephalosporin) (1).
Sternoclavicular (SC) joint septic arthritis is rare, making up only 1% of septic arthritis cases (3,4). IV drug use is the most common predisposing risk factor, present in approximately 20% of cases (4). Infection most commonly occurs secondary to hematogenous seeding, as was likely the cause in our patient (3). Ross and Shamsuddin reviewed 180 cases of SC septic arthritis and found that patients were primarily male (73%) with a mean age of 45 years old (4). Chest pain was the most common chief complaint (78%) and the most common physical exam finding was a tender SC joint, seen in 90% of cases. In the ED, 65% of patients were febrile and only 56% had a leukocytosis. The most common associated risk factor was IV drug use (21%) while diabetes was associated with 13% of cases and a remarkable 23% had no known risk factors. CT imaging of the chest is likely a high yield study in these patients, as this review found that in all 95 patients who had CT imaging performed, a serious complication related to their septic arthritis was found. Complications included osteomyelitis (55%), chest wall abscess (25%), and mediastinitis (13%). Fortunately, functional outcomes were almost always good in these cases after irrigation and treatment. While rare, sternoclavicular septic arthritis should be promptly identified and treated to prevent extension of the infection to surrounding vessels, mediastinum, and pleural space (3).
Learning Points:
· Septic arthritis is a “don’t miss” diagnosis in the emergency department and should be considered in all patients who present with a tender, swollen joint with limited range of motion.
· While large joints are the most common site of septic arthritis, any joint can become infected including less commonly considered sites such as the acromioclavicular and sternoclavicular joints.
· A complete skin exam is essential in all patients with evidence on history and workup of infection. In this case, the patient did not immediately mention the nodule over his sternoclavicular joint until it was seen on physical exam.
· Consider obtaining chest CT for patients with suspected sternoclavicular septic arthritis to look for complications such as chest wall abscess, mediastinitis, or osteomyelitis.
Created By:
Alexandra Atkins, MD.
Emergency Medicine Resident | PGY1
Cook County Emergency Medicine
Reviewed By:
Scott Sherman, M.D.
Associate Program Director | Cook County Emergency Medicine
References:
(1) Burton JH, Fortuna TJ. Joints and Bursae. In: Judith E. Tintinalli, J. Stephan Stapczynski, O. John Ma, Donald M. Yealy, Garth D. Meckler, David M. Cline, ed. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. McGraw-Hill Education; 2016:1927-1932.
(2) Goldenberg DL, Sexton DJ. Septic arthritis in adults. In: UpToDate, Spelman D, Baron EL (ed.), UpToDate, (Accessed 1/29/2022).
(3) Tapscott DC, Benham MD. Sternoclavicular Joint Infection. In: StatPearls. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/pubmed/31869185
(4) Ross JJ, Shamsuddin H. 2004. “Sternoclavicular Septic Arthritis: Review of 180 Cases.” Medicine 83 (3): 139–48. https://doi.org/10.1097/01.md.0000126761.83417.29.