Basic Echocardiography
Learning Objectives:
Describe the indications and limitations of POC Echo
Perform standard POC Echo windows (subcostal, parasternal, and apical) and planes (four chamber, long and short axis)
Identify relevant US anatomy, including the pericardium, cardiac chambers, valves, descending thoracic aorta, and inferior vena cava
Evaluate left ventricular function and central venous pressure to guide hemodynamic assessment of patient
Identify cardiac arrest, pericardial effusions with or without sonographic evidence of tamponade, and dilation of the aortic root or the descending thoracic aorta
Advanced evaluation:
Acquire a view of the aortic arch and recognize aortic arch dissection and/or aneurysm
Identification of right ventricular dysfunction
Assessment of cardiac output and fluid responsiveness
Procedural guidance: ultrasound-guided pericardiocentesis, ultrasound-assisted transvenous pacer placement, and ultrasound-guided central venous catheter placement
Integrate advanced emergency POC echocardiography into individual patient management and departmental function
Indications:
Detection of pericardial effusion with or without sonographic evidence of tamponade
Evaluation of intrinsic cardiac activity in the setting of a cardiac arrest
Evaluation of global left ventricular systolic function
Evaluation of right heart dysfunction
Extended Indications:
Evaluation of volume status and cardiac preload
Identification of acute right ventricular dysfunction in the setting of acute chest pain, dyspnea, or hemodynamic instability
Identification of aortic dissection or thoracic aortic aneurysm
Assessment for volume responsiveness and cardiac output measurements
Procedural guidance for emergent pericardiocentesis, pacemaker wire placement and capture
Integration of POC Echo into cardiac arrest management (identifying pseudo-PEA vs true PEA or asystole, identification of the underlying cause of arrest, utilizing echo findings to help prognosticate likelihood of ROSC or survival to admission and/or hospital discharge)
Required Views:
Parasternal long view showing the right ventricle, left ventricle, left atrium mitral valve, aortic root, and descending aorta.
c/o Kyle Ackerman, MD
Apical 4 Chamber view with the left side of the heart on the right hand of the screen.
c/o Colleen Andrews, MD
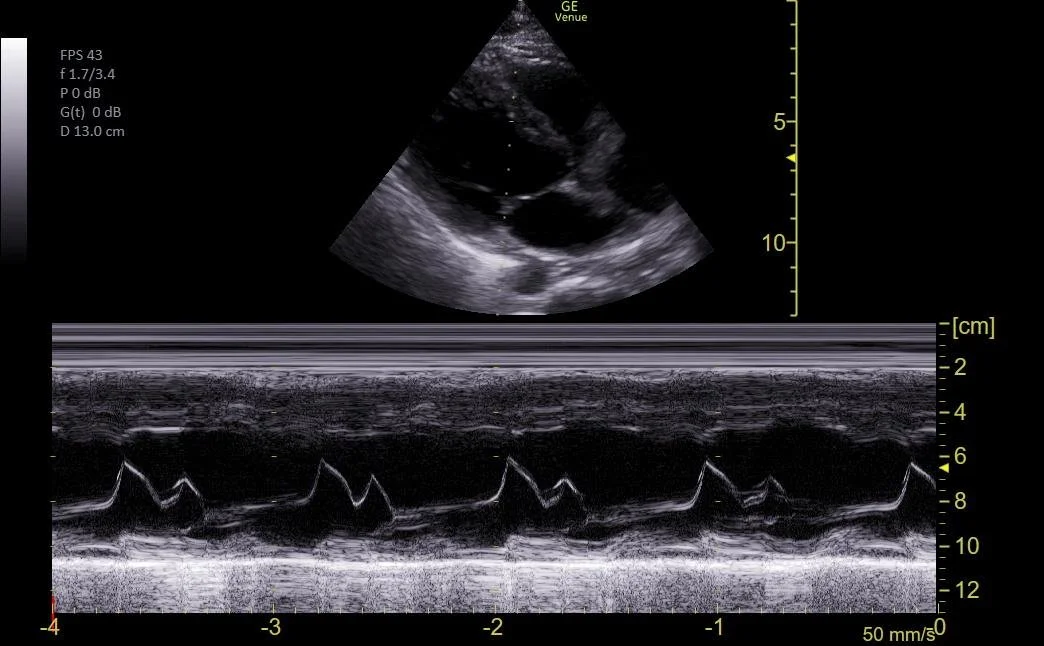
Parasternal long view showing the EPSS (end-point septal separation) using M-Mode through the mitral valve leaflet to evaluate the EF.
c/o VIctoria Gonzalez, MD
Subxiphoid view showing the liver, right ventricle, right atrium, left atrium, and left ventricle.
c/o Kyle Ackerman, MD
Parasternal short view showing the left ventricle and right ventricle at the level of the papillary muscles.
c/o Kyle Ackerman, MD
View of the IVC and hepatic vein leading to the right atrium
c/o Victoria Gonzalez, MD
How to Scan:
ACEP Sonoguide: Cardiac Ultrasound
POCUS 101: Cardiac Ultrasound Made Easy
Tips/Tricks/Pitfalls:
Remember to evalute the “E’s of Echo: Ejection, Effusion, Equality, Entrance (IVC), Exit (Aortic Root)” in every patient
Scan in a systematic pattern to make sure that you visualize every structure every time
The descending thoracic aorta will help differentiate pericardial effusions (will travel anterior to the aorta) from pleural effusions (will dive posterior to the thoracic aorta)
Patients with COPD will often have extremely challenging parasternal views, so start with a subxiphoid view to get a more reliable quick POC echo assessment on a dyspneic patient with known COPD
Pericardial fat pads can mimic pericardial effusions. Check for fluid in dependent areas of the heart as well if you are unsure about a finding
Having a patient lay in left lateral decubitus will often help to optimize views
A sustained inspiration will often improve subxiphoid views while “holding” a breath after a complete exhalation will often improve parasternal views
Pathology:
Parasternal long view demonstrating severely reduced ejection fraction
c/o Ginny Kim, MD
Parasternal long view showing a massively dilated aortic root (7cm) in size.
c/o Emily Zhao, MD
Parasternal short view showing a dilated right ventricle and D-Sign in a patient with a large PE.
c/o Sohaib Amjad, MD
Parasternal long view showing a normal aortic root with a dissection flap in the descending aorta.
c/o Leslie Cachola, MD
Apical-4-Chamber view showing a McConnell’s Sign at the apex of the right ventricle
c/o Jose Reyes, MD
Flat (<1cm) and collapsing (>50%) IVC indicating low intravascular volume.
c/o Sofia Gambuto, MD
Subxiphoid view with pericardial effusion with chamber collapse indicating tamponade.
c/o Susan Mari, MD
Plethoric IVC (>2cm) with minimal collapsiblity (<50%) indicating fluid overload.
c/o David Murray, MD
Key Literature:
Kennedy Hall, M., et al. The “5Es” of emergency physician–performed focused cardiac ultrasound
Patel, Avani R., et al. Cardiac ultrasound in the intensive care unit
Additional Resources:
Malin and Dawson iBook Volume 1, Chapter 2: Basic Echo
ACEP Emergency Ultrasound Imaging Criteria Compendium Pages 6-11
The POCUS Atlas: Echocardiography
AEUS Lecture by Anirudh Ramachandran
Author: Niyi Soetan, MD (Class of 2026)
Reviewed by: David Murray, MD FPD-AEMUS